By Sayer Ji
Contributing Writer for Wake Up World
Millions of asymptomatic women undergo breast screening annually because their doctors tell them to do so. Not only are these women’s presumably healthy breasts being exposed to highly carcinogenic x-rays, but thousands have received a diagnosis of ‘breast cancer’ for entirely benign lesions that, when left untreated, would have caused no harm to them whatsoever – even 20 years later.
A study published in the International Journal of Cancer titled “Is carcinoma in situ a precursor lesion of invasive breast cancer?” is bringing much needed attention to a long standing cancer myth that is harming tens of thousands of women each year: that in situ (non- or slow-growing) breast lesions (carcinoma) inevitably progress to malignant cancers that will cause harm or death if left untreated through conventional methods. This is simply not true.
The 25-year prospective follow-up study measured the probability of development of invasive breast cancer (BC) following the diagnosis of carcinomas in situ (CIS) by linking the Canadian National Breast Screening Study (CNBSS) to cancer registries and a national vital statistics database. CIS was classified into ductal (DCIS) and lobular carcinoma in situ (LCIS).
The study found that while the average time from the diagnosis of CIS to invasive BC was 6.3 years ( ±5.6), and the 20-year cumulative incidence probabilities for DCIS and LCIS were 19.0% (95%CI: 11.2, 26.8) and 21.3% (95%CI: 7.1, 35.4) respectively, at 20-year post CIS diagnosis, more than 80% of them remained free of invasive BC.
Clearly, the notion that DCIS and LCIS always progress to invasive cancer, and therefore must be treated aggressively with the present-day ‘standard of care’ — lumpectomy, mastectomy, radiation, and chemotherapy — is disproved. In other words, the natural history of in situ lesions like DCIS – commonly misidentified by conventional oncologists as ‘cancers’ – indicate they progress to invasive breast cancer only 20% of the time, even after 20 years without treatment.
The study concluded:
“This low probability of developing invasive BC post CIS diagnosis does not support the notion that CIS of the breast is an obligate precursor lesion of invasive BC.”
Even ‘Invasive Breast Cancer’ Is Misunderstood
The misunderstanding about in situ breast lesions extends to so-called ‘invasive breast cancer’ (BC) as well. Whereas invasive BC is considered by the conventional medical establishment as a lethal disease process that must be cut, burned or poisoned out of the body as soon as it is found, there is great heterogeneity within this biological category, including forms with very low (indolent) and high risk for progression and death, and the whole gamut types between.
Also, several years ago, the journal Lancet Oncology found that some clinically verified “invasive” cancers appear to regress with time if left untreated, further complicating matters:
“Because the cumulative incidence among controls did not reach that of the screened group, we believe that many invasive breast cancers detected by repeated mammography screening do not persist to be detected by screening at the end of 6 years, suggesting that the natural course of many of the screen-detected invasive breast cancers is to spontaneously regress.” [emphasis added]
The present inability of the conventional medical system to identify any clear method to determine the difference between a benign, malignant, or possibly regression-prone form of BC, puts the patient at profound risk of overdiagnosis and overtreatment, the consequences of which can be devastating. The lack of individualized treatment and informed choice leads many women to undergo treatment who may have never experienced disease progression had they chosen to employ watchful waiting, or alternative approaches.
The Larger Issue: ‘Cancer’ Has Been Completely Misunderstood To The Detriment of Millions
A 2013 study published in JAMA titled, “Overdiagnosis and Overtreatment in Cancer: An Opportunity for Improvement,”[1] explains that the word cancer is highly misunderstood and misused. It has become clear that after 30 years of cancer screening with an emphasis on ‘detecting cancer early’, the goals of such campaigns to reduce the rate of late-stage disease and decrease cancer mortality has clearly not been realized. [See video for an in-depth explanation.] This would not happen if the exponential increase of diagnoses and treatment for ‘early stage’ cancer produced as a result of mammography screening over the past 25 years were actually finding ‘cancers,’ and not so-called indolent lesions of epithelial origin – i.e. benign lesions that will not progress to malignancy.
The study expanded on these implications:
“What has emerged has been an appreciation of the complexity of the pathologic condition called cancer. The word “cancer” often invokes the specter of an inexorably lethal process; however, cancers are heterogeneous and can follow multiple paths, not all of which progress to metastases and death, and include indolent disease that causes no harm during the patient’s lifetime. Better biology alone can explain better outcomes.”
“Use of the term “cancer” should be reserved for describing lesions with a reasonable likelihood of lethal progression if left untreated. There are 2 opportunities for change. First, premalignant conditions (e.g., ductal carcinoma in situ or high-grade prostatic intraepithelial neoplasia) should not be labeled as cancers or neoplasia, nor should the word “cancer” be in the name. Second, molecular diagnostic tools that identify indolent or low-risk lesions need to be adopted and validated. Another step is to reclassify such cancers as IDLE (indolent lesions of epithelial origin) conditions.”
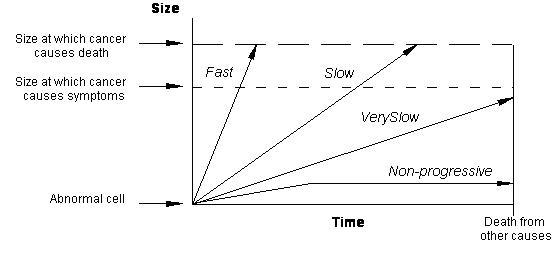
Fundamentally, overdiagnosis results from the fact that screen-detected ‘cancers’ are disproportionately slower growing ones, present with few to no symptoms, and would never progress to cause harm if left undiagnosed and untreated. The figure below depicts four arrows representing four types of abnormal cell growth: 1) Fast 2) Slow 3) Very Slow 4) Non-Progressive.
Unless the abnormal cell growth reaches a size at which cancer symptoms occur, it is not justifiable to treat it; nor is it appropriate to call it ‘cancer,’ as technically it is an indolent or benign lesion. Faster growing cells can contribute to symptoms over a life time, but even then, that does not mean that it will necessarily progress to cause death before natural or other causes take the patients life. In fact, premature treatment can greatly reduce the quality and length of life due to the side effects of chemotherapy, radiation, surgery, and the added stress and psychospiritual trauma of receiving a diagnosis.
The Implications of this Cancer Reclassification to the Healthy and ‘Cancer Survivors’
There are two primary implications of this reclassification of ‘cancer.’
First, those undergoing ‘preventive’ cancer screening need to be aware of how frequently overdiagnosis occurs (up to 50% within 10 years), especially in breast, lung, prostate and thyroid ‘cancers’– the most prevalent lesions overdiagnosed through routine screening, and indiscriminately treated regardless of differing risk stratifications. For instance, before the advent of mammography, only 3% of detected breast cancer were identified as DCIS.[2] Today, more than one-third of screen-detected early cancers are DCIS, with the unfortunate result that 33% of those diagnosed with DCIS receiving breast removal (mastectomy), 48% receiving lumpectomy and radiation treatments, 16% receiving lumpectomy, and only 3% electing to do nothing.[3]
The fact that DCIS will do no harm in at least 80% of the time reveals a great burden of iatrogenic harm is being borne by women who are being coerced by an outdated treatment model that is no longer sufficiently evidence-based.
Second, there are now millions of formerly screened, and subsequently treated, patients who had indolent lesions of epithelial origin, such as DCIS, LCIS, or in the case of men, high grade intraepithelial hyperplasia (HGIH) (‘prostate cancer’), whose diagnoses were invalid and should never have been treated. For instance, it has been estimated that 1.3 million women were falsely diagnosed with and treated for ‘breast cancer’ in the past 30 years. These patients believe they are ‘cancer’ survivors, when in fact they are surviving the psychospiritual and physical traumas and abuses of their treatments and not their ‘disease.’
While not knowing the truth may be considered somewhat protective against further trauma associated with no longer identifying with the aggressor – i.e. the conventional medical model – and the potentially devastating realization that they have succumbed to disfigurement and poisoning from unnecessary treatments, continuing marketing campaigns (such as Breast Cancer Awareness Month; Pink Ribbons; Race for the Cure) encourage ‘survivors’ to act as brand ambassadors for breast cancer associated products and services, drawing other otherwise healthy women into receiving unnecessary and/or dangerous diagnoses and treatments generated by screening programs.
This process I have described in the context of the breast cancer industry ‘memeplex’, which I presented on in Washington in 2013 at the Mind-Body Week Conference. You can watch part of my lecture here.
Moving the Paradigm Forward
Over the past few years, a number of studies have been published revealing a paradigm shift in our understanding of cancer. Some of these findings reveal:
- Many screen-detected cancers are benign lesions
- Overdiagnosis and overtreatment is rampant, and represents a profound burden of medicine-caused (iatrogenic) harm
- The natural history of some cancers is to spontaneously regress
- Diagnostic technologies like mammography are likely contributing to new cancers
- Radiation therapy (radiotherapy) can dramatically increase cancer cell malignancy
- Chemotherapy increases highly tumoriogenic cancer stem cell populations
- False positives can have long-lasting adverse psychospiritual effects
- Cancer diagnoses can increase the risk of heart-related deaths by up to 26 fold within the first week following diagnoses
- Cancer has been completely misunderstood; it is a survival mechanisms unmasked
For additional research on natural/integrative cancer treatments and the unintended, adverse effects of conventional ones, view the following health guides on Greenmedinfo.com:
- Health Guide: Cancer Research
- Health Guide: Breast Cancer Research
Resources:
[1] Laura Esserman, MD, MBA, et al. Overdiagnosis and Overtreatment in Cancer: An Opportunity for Improvement JAMA 2013
[2] Laura Esserman, MD, MBA; and Michael Alvarado, MD. Setting a Research Agenda for Ductal Carcinoma In Situ That Meets the Current Need for Change Ann Intern Med. 2014;160(7):511-512. doi:10.7326/M14-0435
[3] IBID
Updated September 2014
Further articles by Sayer Ji:
- Splenda Found To Have Possible Neurotoxic Properties In Animal Study
- Research: Curcumin Is A Triple Negative Breast Cancer Killer
- The Spice That Prevents Fluoride From Destroying Your Brain
- Turmeric Beats Ibuprofen for Arthritis of the Knee
- Live Flu Vaccines Increase Infectious Bacteria Counts 100-Fold in Mice
- FAIL: Another Mammography Study Finds They Don’t Save Lives
- MSG Proven Highly Toxic: 1 Dose Causes Headache In Healthy Subjects
- Black Seed Extract ‘Cures’ HIV Patient Naturally
- The Cancer-Causing Metal Millions Eat, Wear or Have Injected Into Their Kids
- Biophotons: The Human Body Emits, Communicates with, and is Made from Light
- The 2013 Measles Outbreak: A Failing Vaccine, Not A Failure To Vaccinate
- 3 Evidence-Based Ways To Reverse Skin Aging Naturally
- How to Clean Your Arteries With One Simple Fruit
- 13 Evidence-Based Medicinal Properties of Coconut Oil
About the author:
 Sayer Ji is an author, educator, Steering Committee Member of the Global GMO Free Coalition (GGFC), advisory board member of the National Health Federation, and the founder of GreenMedInfo.com – an open access, evidence-based resource supporting natural and integrative modalities. His writings have been published and referenced widely in print and online, including Truthout, Mercola.com, The Journal of Gluten Sensitivity, New York Times and The Well Being Journal.
Sayer Ji is an author, educator, Steering Committee Member of the Global GMO Free Coalition (GGFC), advisory board member of the National Health Federation, and the founder of GreenMedInfo.com – an open access, evidence-based resource supporting natural and integrative modalities. His writings have been published and referenced widely in print and online, including Truthout, Mercola.com, The Journal of Gluten Sensitivity, New York Times and The Well Being Journal.
In 1995 Sayer received a BA degree in Philosophy from Rutgers University, where he studied under the American philosopher Dr. Bruce W. Wilshire, with a focus on the philosophy of science. In 1996, following residency at the Zen Mountain Monastery in upstate New York, he embarked on a 5 year journey of service as a counsellor-teacher and wilderness therapy specialist for various organizations that serve underprivileged and/or adjudicated populations. Since 2003, Sayer has served as a patient advocate and an educator and consultant for the natural health and wellness field.
Visit GreenMedInfo online and on Facebook, or sign up for GreenMedInfo’s Newsletter,
Disclaimer: This article is not intended to provide medical advice, diagnosis or treatment.
If you've ever found value in our articles, we'd greatly appreciate your support by purchasing Mindful Meditation Techniques for Kids - A Practical Guide for Adults to Empower Kids with the Gift of Inner Peace and Resilience for Life.
In the spirit of mindfulness, we encourage you to choose the paperback version. Delve into its pages away from screen glare and notifications, allowing yourself to fully immerse in the transformative practices within. The physical book enriches the learning process and serves as a tangible commitment to mindfulness, easily shared among family and friends.
Over the past few years, Wake Up World has faced significant online censorship, impacting our financial ability to stay online. Instead of soliciting donations, we're exploring win-win solutions with our readers to remain financially viable. Moving into book publishing, we hope to secure ongoing funds to continue our mission. With over 8,500 articles published in the past 13 years, we are committed to keeping our content free and accessible to everyone, without resorting to a paywall.