February 15th, 2018
By Sayer Ji
Contributing writer for Wake Up World
What if everything your doctor told you about osteoporosis and osteopenia was wrong?
What if osteoporosis was not the primary cause of fractures in aging populations? What if both the definitions of osteoporosis and osteopenia used to justify pharmaceutical treatment were both misleading and age inappropriate?
These are questions we explored in a previous exposé, titled “Osteoporosis Myth: The Dangers of High Bone Mineral Density“, wherein we explored evidence showing the so-called “osteoporosis epidemic” is not an evidence-based concept but a manufactured one designed to serve the interests of a growing industrial medical/pharmaceutical complex.
[pro_ad_display_adzone id=”110028″]
A paper published in the Journal of Internal Medicine, titled “Osteoporosis: the emperor has no clothes“, confirms that the primary cause of what are normally labeled “osteoporotic fractures” are falls and related modifiable lifestyle factors and not osteoporosis, i.e. abnormally “porous” or low-density bones.
The new study pointed out three false notions that can be disputed:
-
Mistaken pathophysiology: “Most fracture patients have fallen, but actually do not have osteoporosis. A high likelihood of falling, in turn, is attributable to an ageing-related decline in physical functioning and general frailty.”
-
Ineffective screening: “Currently available fracture risk prediction strategies including bone densitometry and multifactorial prediction tools are unable to identify a large proportion of patients who will sustain a fracture, whereas many of those with a high fracture risk score will not sustain a fracture.”
-
Unproven and unsafe treatment: “The evidence for the viability of bone-targeted pharmacotherapy in preventing hip fracture and other clinical fragility fractures is mainly limited to women aged 65–80 years with osteoporosis, whereas the proof of hip fracture-preventing efficacy in women over 80 years of age and in men at all ages is meagre or absent. Further, the antihip fracture efficacy shown in clinical trials is absent in real-life studies. Many drugs for the treatment of osteoporosis have also been associated with increased risks of serious adverse events. There are also considerable uncertainties related to the efficacy of drug therapy in preventing clinical vertebral fractures, whereas the efficacy for preventing other fractures (relative risk reductions of 20–25%) remains moderate, particularly in terms of the low absolute risk reduction in fractures with this treatment”
The open access study is well worth reading in its entirety, but below are a few takeaways that we want to highlight.
Falling and Not Low Bone Mineral Density Is The Primary Cause of Fractures
Millions of men and women whose bones are actually normal for their age group (Z-score) are being manipulated into thinking that their bones should remain as dense as an approximately 30-year-old young adult (T-score) despite the natural process of bone thinning and reduction of density that attends the aging process. This T-score based bone density system pathologizes/over-medicalizes normal bone density variations, creating disease diagnoses where none should be found — a situation that is incredibly lucrative from the perspective of the bottom line of pharmaceutical and medical services companies. This has lead to a massive problem with overdiagnosis and overtreatment — two euphemistic technical terms to describe what happens when asymptomatic and otherwise healthy populations are told they have a ‘specific disease’ that they do not have (overdiagnosis), and subsequently pressured into taking pharmaceuticals (overtreatment), whose adverse effects often contribute to morbidity and premature mortality.
The reality, however, is that falling — not low bone mineral density — is the primary reason why fractures occur. Since it is a statistical fact that the older you get the more often you fall, and since the older you get the less dense your bones become, it is easy to confuse the lower bone mineral density as a “cause” and not just an “association” with increased fracture risk. The authors of the new study provided this clever cartoon to drive the point home:
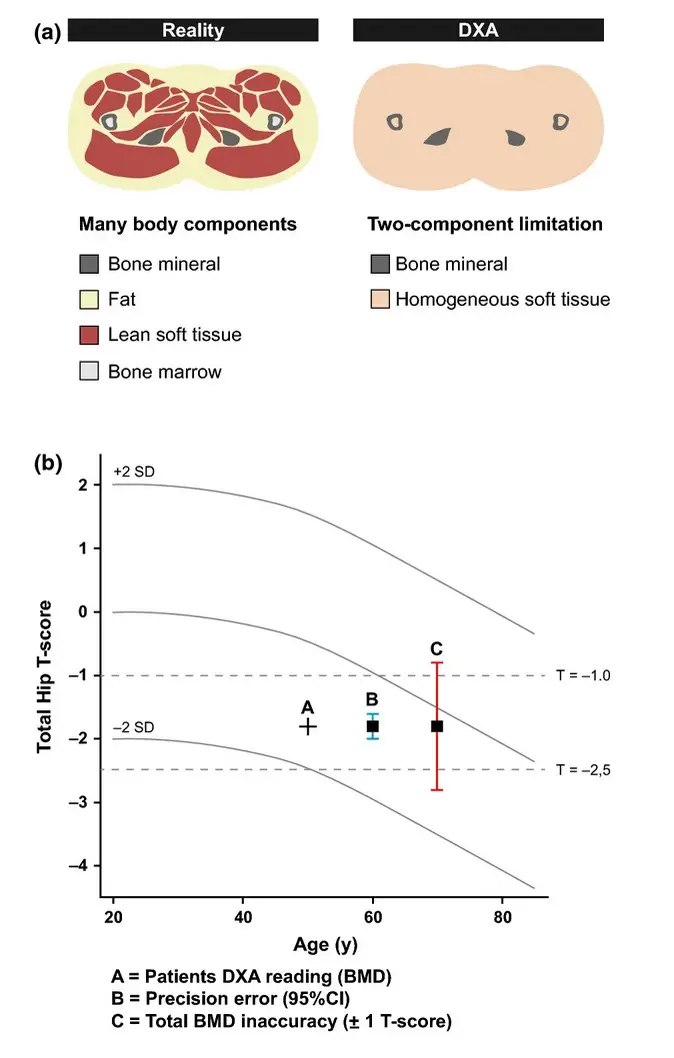
Given the reality behind what causes (and prevents) fracture, exercise and its resultant muscular and neurological health effects are of vital importance when it comes to minimizing the risk of falls, as well as surviving them without a fracture. And yet the reality is that the x-ray based DXA scans used to ascertain bone density do nothing but determine the density of the skeletal system, and not bone quality, i.e. strength. Nor can the DXA scan ascertain the structure/function (and therefore health) of the other tissues within the body that directly contribute to determining the risk of falling and the effects that the impact of a fall will have on the skeletal system. The following diagram shows the discrepancy that emerges between reality and the DXA image:
Where is the Evidence for Pharmaceutical “Prevention” of Fracture?
While anti-resportive bone drugs like Fosamax (a bisphosphonate) may contribute to increased bone mineral density, they do not necessarily improve bone quality and strength. Very dense bone created by destroying osteoclasts (bone-degrading cells) may be far more brittle than less dense bone where there is healthy turnover of the osteoclasts and osteoblasts (bone-building cells). In fact, drugs like Fosamax are notorious for contributing to bone degeneration in the jawbone (osteonecrosis). Also, we have discovered an extensive body of research indicating higher-than-normal bone density greatly increases the risk of malignant breast cancer, further calling into question the present day fixation on increasing bone density at any cost with highly toxic calcium supplements and drugs. Moreover, the new study points out that meta-analyses of the clinical literature on pharmacological treatment of osteoporosis for fracture risk reduction have produced almost no supportive evidence. Despite this, they point out that, “Osteoporosis guidelines systematically ignore the obvious ‘evidence void’ in the RCTs.”
The authors conclude: “Given all this, should ‘osteoporosis’ be added to a long list of diagnoses for which doing less, or even nothing, is better than our contemporary practice?”
Thankfully, we don’t just have to “do nothing.” Exercise, nutrition, and practices like yoga, tai chi, etc., can go a long way to reduce the risk of fracture, as well as supporting healthy bone mineral density, and more importantly, bone strength and structural integrity.
The Manufacturing of Bone Diseases: The Story of Osteoporosis and Osteopenia
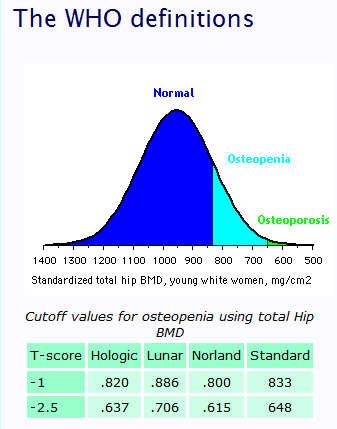
The present-day definitions of Osteopenia and Osteoporosis were arbitrarily conceived by the World Health Organization (WHO) in the early 90’s and then projected upon millions of women’s bodies seemingly in order to convince them they had a drug-treatable, though symptomless, disease.
Osteopenia (1992)[i] and Osteoporosis (1994)[ii] were formally identified as skeletal diseases by the WHO as bone mineral densities (BMD) 1 and 2.5 standard deviations, respectively, below the peak bone mass of an average young adult Caucasian female, as measured by an x-ray device known as Dual energy X-ray absorptiometry (DXA, or DEXA). This technical definition, now used widely around the world as the gold standard, is disturbingly inept, and as we shall see, likely conceals an agenda that has nothing to do with the promotion of health.
Deviant Standards: Aging Transformed Into a Disease
A ‘standard deviation’ is simply a quantity calculated to indicate the extent of deviation for a group as a whole, i.e. within any natural population there will be folks with higher and lower biological values, e.g. height, weight, bone mineral density, cholesterol levels. The choice of an average young adult female (approximately 30-year old) at peak bone mass in the human lifecycle as the new standard of normality for all women 30 or older, was, of course, not only completely arbitrary but also highly illogical. After all, why should a 80-year old’s bones be defined as “abnormal” if they are less dense than a 30-year old’s?
Within the WHO’s new BMD definitions the aging process is redefined as a disease, and these definitions targeted women, much in the same way that menopause was once redefined as a “disease” that needed to be treated with synthetic hormone replacement (HRT) therapies; that is, before the whole house of cards collapsed with the realization that by “treating” menopause as a disease the medical establishment was causing far more harm than good, e.g. heart disease, stroke and cancer.
As if to fill the void left by the HRT debacle and the disillusionment of millions of women, the WHO’s new definitions resulted in the diagnosis, and subsequent labeling, of millions of healthy middle-aged and older women with what they were now being made to believe was another “health condition,” serious enough to justify the use of expensive and extremely dangerous bone drugs (and equally dangerous mega-doses of elemental calcium) in the pursuit of increasing bone density by any means necessary.
One thing that cannot be debated, as it is now a matter of history, is that this sudden transformation of healthy women, who suffered no symptoms of “low bone mineral density,” into an at-risk, treatment-appropriate group, served to generate billions of dollars of revenue for DXA device manufacturers, doctor visits, and drug prescriptions around the world.
WHO Are They Kidding?
Osteopenia is, in fact, a medical and diagnostic non-entity. The term itself describes nothing more than a statistical deviation from an arbitrarily determined numerical value or norm. According to the osteoporosis epidemiologist Dr. L. Joseph Melton at the Mayo Clinic who participated in setting the original WHO criteria in 1992, “[osteopenia] was just meant to indicate the emergence of a problem,” and noted that “it didn’t have any particular diagnostic or therapeutic significance. It was just meant to show a huge group who looked like they might be at risk.”[iii] Another expert, Michael McClung, director of the Oregon Osteoporosis Center, criticized the newly adopted disease category osteopenia by saying ”We have medicalized a nonproblem.”[iv]
In reality, the WHO definitions violate both commonsense and fundamental facts of biological science (sadly, an increasingly prevalent phenomenon within drug company-funded science). After all, anyone over 30 years of age should have lower bone density than a 30 year old, as this is consistent with the normal and natural healthy aging process. And yet, according to the WHO definition of osteopenia, the eons-old programming of our bodies to gradually shed bone density as we age, is to be considered a faulty design and/or pathology in need of medical intervention.
How the WHO, or any other organization which purports to be a science-based “medical authority,” can make an ostensibly educated public believe that the natural thinning of the bones is not normal, or more absurdly: a disease, is astounding. In defense of the public, the cryptic manner in which these definitions and diagnoses have been cloaked in obscure mathematical and clinical language makes it rather difficult for the layperson to discern just how outright insane the logic they are employing really is.
So, let’s look closer at the definitions now, which are brilliantly elucidated by Washington.edu’s published online course on Bone Densitometry, which can viewed in its entirety here.
The Manufacture of a Disease through Categorical Sleight-of-Hand
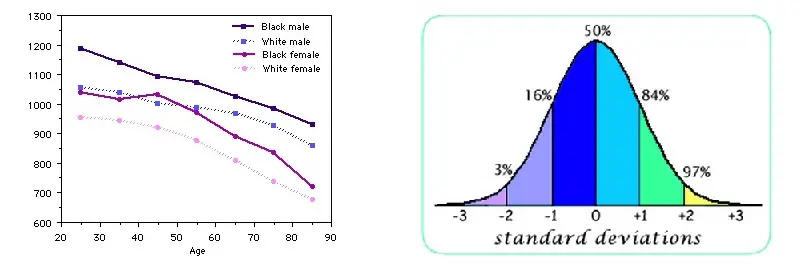
This image on the left below shows the natural decrease in hip bone density occurring with age, with variations in race and gender depicted. Observe that loss of bone mineral density with age is a normal process.
On the right is the classical bell-shaped curve, from which T- and Z-scores are based.
T-scores are based on the young adult standard (30-year old) bone density as being normal for everyone, regardless of age, whereas the much more logical Z-score compares your bone mineral density to that of your age group, as well as sex and ethnic background.
Now here’s where it gets disturbingly clear how ridiculous the T-score really system is….
This image shows how within the population of women used to determine “normal” bone mineral density, e.g. 30-year olds, 16% of them already “have” osteopenia” according to the WHO definitions, and 3% already “have” osteoporosis!
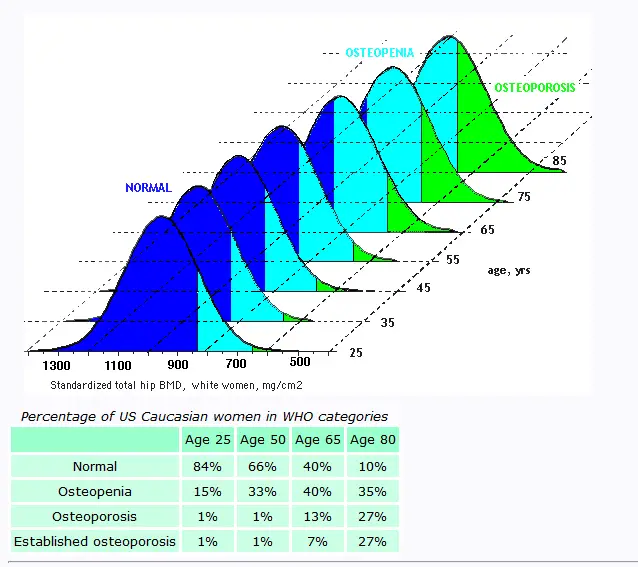
According to the Washington.edu online course “one standard deviation is at the 16th percentile, so by definition 16% of young women have osteopenia! As shown below, by the time women reach age 80, very few are considered normal.”
Below you will see what happens when the WHO definitions of “normal bone density” are applied to aging populations. Whereas at age 25, 15% of the population will “have” osteopenia, by age 50 the number grows to 33%. And by age 65, 60% will be told they have either osteopenia (40%) or osteoporosis (20%).
On the other hand, if one uses the Z-score, which compares your bones to that of your age group, something remarkable happens: a huge burden of “disease” disappears! In a review on the topic published in 2009 in the Journal of Clinical Densitometry, 30-39% of the subjects who had been diagnosed with osteoporosis with two different DXA machine models were reclassified as either normal or “osteopenic” when the Z- score was used instead of the T-score. The table therefore can be turned on the magician-like sleight-of-hand used to convert healthy people into diseased ones, as long as an age-appropriate standard of measurement is applied, which presently it is not.
Bone Mineral Density is NOT Equivalent to Bone Strength
As you can see there are a number of insurmountable problems with the WHO’s definitions, but perhaps the most fatal flaw is the fact that the Dual energy X-ray absorpitometry device (DXA) is only capable of revealing the mineral density of the bone, and this is not the same thing as bone quality/strength.
While there is a correlation between bone mineral density and bone quality/strength – that is to say, they overlap in places — they are not equivalent. In other words, density, while an excellent indicator of compressive strength (resisting breaking when being crushed by a static weight), is not an accurate indicator of tensile strength (resisting breaking when being pulled or stretched).
Indeed, in some cases having higher bone density indicates that the bone is actually weaker. Glass, for instance, has high density and compressive strength, but it is extremely brittle and lacks the tensile strength required to withstand easily shattering in a fall. Wood, on the other hand, which is closer in nature to human bone than glass or stone is less dense relative to these materials, but also extremely strong relative to them, capable of bending and stretching to withstand the very same forces which the bone is faced with during a fall. Or, take spider web. It is has infinitely greater strength and virtually no density. Given these facts, having “high” bone density (and thereby not having osteoporosis) may actually increase the risk of fracture in a real-life scenario like a fall.
Essentially, the WHO definitions distract from key issues surrounding bone quality and real world bone fracture risks, such as gait and vision disorders.[v] In other words, if you are able to see and move correctly in our body, you are less likely to fall, which means you are less prone to fracture. Keep in mind also that the quality of human bone depends entirely on dietary and lifestyle patterns and choices, and unlike x-ray-based measurements, bone quality is not decomposable to strictly numerical values, e.g. mineral density scores. Vitamin K2 and soy isoflavones, for instance, significantly reduce bone fracture rates without increasing bone density. Scoring high on bone density tests may save a woman from being intimidated into taking dangerous drugs or swallowing massive doses of elemetal calcium, but it may not translate into preventing “osteoporosis,” which to the layperson means the risk of breaking a bone.
But high bone mineral density may result in far worse problems…
High Bone Mineral Density and Breast Cancer
One of the most important facts about bone mineral density, conspicuously absent from discussion, is that having higher-than-normal bone density in middle-aged and older women actually INCREASES their risk of breast cancer by 200-300%, and this is according to research published in some of the world’s most well-respected and authoritative journals, e.g. Lancet, JAMA, NCI. (see citations below).
[pro_ad_display_adzone id=”110030″]
While it has been known for at least fifteen years that high bone density profoundly increases the risk of breast cancer — and particularly malignant breast cancer — the issue has been given little to no attention, likely because it contradicts the propaganda expounded by mainstream woman’s health advocacy organizations. Breast cancer awareness programs focus on x-ray based breast screenings as a form of “early detection,” and the National Osteoporosis Foundation’s entire platform is based on expounding the belief that increasing bone mineral density for osteoporosis prevention translates into improved quality and length of life for women.
The research, however, is not going away, and eventually these organizations will have to acknowledge it, or risk losing credibility altogether.
- Journal of the American Medical Association (1996): Women with bone mineral density above the 25th percentile have 2.0 to 2.5 times increased risk of breast cancer compared with women below the 25th percentile.
- Journal of Nutrition Reviews (1997): Postmenopausal women in the highest quartile for metacarpal bone mass were found to have an increased risk of developing breast cancer, after adjusting for age and other variables known to influence breast cancer risk.
- American Journal of Epidemiology (1998): Women with a positive family history of breast cancer and who are in the highest tertile bone mineral density are at a 3.41-fold increased risk compared with women in the lowest tertile.
- Journal of the National Cancer Institute (2001): Elderly women with high bone mineral density (BMD) have up to 2.7 times greater risk of breast cancer, especially advanced cancer, compared with women with low BMD.
- Journal Breast (2001): Women in the lowest quartile of bone mass appear to be protected against breast cancer.
- Journal Bone (2003): Higher bone density (upper 33%) is associated with a 2-fold increased risk of breast cancer.
- European Journal of Epidemiology (2004): Women with highest tertile bone mineral density (BMD) measured at the Ward’s triangle and at the femoral neck are respectively at 2.2-and 3.3-fold increased risk of breast cancer compared with women at the lowest tertile of BMD.
You can view additional citations at GreenMedInfo’s breast cancer-bone density page.
High Bone Density: More Harm Than Good
The present-day fixation within the global medical community on “osteoporosis prevention” as a top women’s health concern, is simply not supported by the facts. The #1 cause of death in women today is heart disease, and the #2 cause of death is cancer, particularly breast cancer, and not death from complications associated with a bone fracture or break. In fact, in the grand scheme of things osteoporosis or low bone mineral density does not even make the CDC’s top ten list of causes of female mortality. So, why is it given such a high place within the hierarchy of women’s health concerns? Is it a business decision or a medical one?
Regardless of the reason or motive, the obsessive fixation on bone mineral density is severely undermining the overall health of women. For example, the mega-dose calcium supplements being taken by millions of women to “increase bone mineral density” are known to increase the risk of heart attack by between 24-27%, according to two 2011 meta-analyses published in Lancet, and 86% according to a more recent meta-analysis published in the journal Heart. Given the overwhelming evidence, the 1200+ mgs of elemental calcium the National Osteoporosis Foundation (NOF) recommends women 50 and older take to “protect their bones,” may very well be inducing coronary artery spasms, heart attacks and calcified arterial plaque in millions of women. Considering that the NOF name calcium supplement manufacturers Citrical and Oscal as corporate sponsors, it is unlikely their message will change anytime soon.
Now, when we consider the case of increased breast cancer risk linked to high bone mineral density, being diagnosed with osteopenia or osteoporosis would actually indicate a significantly reduced risk of developing the disease. What is more concerning to women: breaking a bone (from which one can heal), or developing breast cancer? If it is the latter, a low BMD reading could be considered cause for celebration and not depression, fear and the continued ingestion of inappropriate medications or supplements, which is usually the case following a diagnosis of osteopenia or osteoporosis.
We hope this article will put to rest any doubts that the WHO’s fixation on high bone density was designed not to protect or improve the health of women, but rather to convert the natural aging process into a blockbuster disease, capable of generating billions of dollars of revenue.
To learn more use GreenMedInfo’s natural osteoporosis prevention and treatment database to explore study abstracts and articles relevant to this topic.
References:
- [i] WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland) (2003). “Prevention and management of osteoporosis : report of a WHO scientific group” (PDF). Retrieved 2007-05-31.
- [ii] WHO (1994). “Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group”. World Health Organization technical report series 843: 1–129. PMID 7941614.
- [iii] Kolata, Gina (September 28, 2003). “Bone Diagnosis Gives New Data But No Answers”. New York Times.
- [iv] Ibid
- [v] P Dargent-Molina, F Favier, H Grandjean, C Baudoin, A M Schott, E Hausherr, P J Meunier, G Bréart Fall-related factors and risk of hip fracture: the EPIDOS prospective study. Lancet. 1996 Jul 20;348(9021):145-9. PMID: 8684153
Recommended articles by Sayer Ji:
- The Powerful Aspirin Alternative Your Doctor Never Told You About
- 13 Evidence-Based Medicinal Properties of Coconut Oil
- Group Drumming Better Than Prozac, Study Suggests
- 25 Cancer Stem-Cell Killing Foods That Are Smarter Than Chemo and Radiation
- Ibuprofen Can Stop Your Heart – 31% Increase in Cardiac Arrest Risk
- How Pomegranate Puts Chemo and Radiation to Shame
- Dramatic Recovery in Parkinson’s Patient with Gluten Free Diet
About the author:

Sayer Ji is the founder of Greenmedinfo.com, a reviewer at the International Journal of Human Nutrition and Functional Medicine, Co-founder and CEO of Systome Biomed, Vice Chairman of the Board of the National Health Federation, and Steering Committee Member of the Global Non-GMO Foundation.
For more, visit GreenMedInfo.com and Facebook.com/GreenMedInfo, or sign up for GreenMedInfo’s free e-Newsletter.
© June 29th 2017 and November 18th 2017 GreenMedInfo LLC. This work is reproduced and distributed with the permission of GreenMedInfo LLC. Want to learn more from GreenMedInfo? Sign up for their newsletter here.
[pro_ad_display_adzone id=”110027″]