Contributing Writer for Wake Up World
A simple remedy to cure infections used back in the days is really not enough anymore in modern times! Today we have to deal with “leaky gut” (intestinal impermeability), low levels of beneficial gut flora, antibiotic resistance, overgrowth of gastrointestinal pathogens and low immunity to disease, to name just a few of the conditions which make the process of healing so much more complex and chronic infections hard to eradicate. This is the end result of the “modern living”, full of toxic, processed foods, heavy pollutants, genetically modified organisms and over medication.
So why exactly can’t we get rid of chronic infections after diligently following the recommended course of remedies? One important contributing factor is the BIOFILM formation.
What Are The Biofilms?
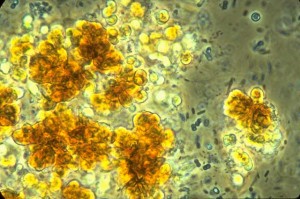
A biofilm is a thin layer of microorganisms that adhere to the surface of an organic or inorganic structure, together with their secreted polymers. Microbes residing within biofilms may consist of one or more species that communicate and collaborate with one another in a heterogeneous community. Biofilms are the predominant phenotype of nearly all bacteria in their natural habitat, whether pathogenic or environmental.
[pro_ad_display_adzone id=”110028″]
They always existed. And they also exist in your intestines, making pathogens harder to eradicate. How does this happen?
Life within a biofilm confers significant survival advantages to bacteria and yeasts. Biofilms strongly adhere to interfaces and resist dislodgement.
Biofilm-residing microorganisms are highly resistant to the spectrum of antimicrobials ranging from germicides and disinfectants to antibiotics and bacteriocins produced by probiotics, as well as to host immunity.
Biofilms have demonstrated the ability to persist in 100 to 1000 times the concentrations of antibiotics and biocides that can inhibit planktonic cells. Pretty hard to break down, don’t you think?
The diversity of the biofilm allows adaptation to overcome multiple stresses and to survive most sequential therapies.
Concomitant therapies that not only attempt to eradicate bacteria, but also affect the biofilm’s community structure and communications may prove more effective than a single or sequential strategy such as antibacterial or antifungal therapy.
Because of molecular methods, science now has the ability to detect biofilms and understand the implications of interspecies chaos that contribute to chronic infections.
Some Of The Infections Related To Biofilms
It is estimated that up to 80% of all human infections have biofilm involvement. These infections range from urinary tract infections, middle-ear infections, cystic fibrosis, dental plaque, chronic skin infections, many chronic diseases, gastrointestinal infections and coatings on indwelling devices such as joint replacement, catheters, cardiac valves, and contact lenses.
Bacterial and fungal pathogens known to reside in biofilms include Escherichia coli, Candida albicans, Clostridium difficile, Clostridium perfringens, Helicobacter pylori, Klebsiella pneumoniae, Legionella pneumophila, Listeria monocytogenes, Pseudomonas aeruginosa, Salmonella typhimurium, Staphylococcus aureus, Staphylococcus epidermidis, and Vibrio cholerae.
Gastrointestinal System
Among the more important species involved in gastrointestinal biofilm formation are Bacteroides, Bifidobacterium, and Fusobacterium. Fusobacterium species appear to play a key role in formation and maintenance of healthy biofilm. However, Fusobacterium can contribute to pathogenic biofilms because it requires association with an aerobic species in certain environments and hence promotes Helicobacter pylori biofilm on the gastric mucosa associated with gastric ulcers. Disrupted healthful biofilm permits colonization and biofilm formation by potential pathogens such as Klebsiella pneumoniae, Escherichia coli, and Candida albicans.
In candida overgrowth, the yeast colonies can dig deep into intestinal walls, damaging the bowel wall in their colonization. Candida colonization occurs within mucosal and skin biofilms where it is highly resistant to eradication.
Teeth
Perhaps the most commonly encountered biofilm disease is dental plaque, and the Streptococcus mutans biofilm leading to cavities.
Typically dental biofilms consist of bacteria that are considered normal oral flora and usually are kept in balance by normal dental hygiene, the other cohabitating bacteria and a good nutrition for the teeth. However the population dynamics and members of these biofilms may change and induce conditions where tooth decay, gingivitis, and other oral health problems may arise. Where dental health is concerned, it is synonymous with biofilms.
Chronic Sinus and Inner Ear Infections
Symptoms of chronic rhinosinusitis (sinus infections) and otitis media (inner ear infections) may be due to a persistent biofilm-based infection that the body fails to fully eliminate. Continual aggravation by these infections may produce lasting, disrupting, and damaging effects.
How To Break Down Biofilms Residing In The Intestines?
Disruption of the healthy gastrointestinal biofilm facilitates an inflammatory response to normal microflora and compromises host defenses against a variety of pathogens. A nonpharmaceutical approach to biofilm eradication involves the use of specific enzymes and binding agents (such as the Interfase supplement by Klaire Labs), probiotics, gut healing supplements, concomitant with antifungals, antiparasitic and/or antibacterial substances and a right customized diet, which supports all metabolic functions.
Article Sources
http://endoexperience.com/userfiles/file/Biofilm_JAMA_Wolcott_and_Ehrlich_2008.pdf
Lewis K. Persister cells, dormancy and infectious disease. Nat Rev Microbiol.
2007;5(1):48-56
InterFase ®: Specialized Enzymes Disrupt Biofilm Matrix
that Embeds Potential Gastrointestinal Pathogens. – Klaire Labs
http://www.frylabs.com/biofilm.php
https://www.protherainc.com/images/prod/brochures/K-INT_Brochure.pdf
https://www.protherainc.com/DisplayDoc.asp
Wolcott, William. CANDIDA ALBICANS . . .Are You Winning Battles But Losing the War?
Stephen Olmstead, MD, Dennis Meiss, PhD, and Janet Ralston, BS. Fungal-Type Dysbiosis & Chronic Disease Exploring The Nature of the Yeast Connection
Recommended articles by Raluca Schachter:
- Vitamin D Supplementation: This is Why It Can Be Wrong
- Hypothyroidism or Hashimoto’s? What You Need to Know and Why It Matters
- Understanding Cannabis Oil
- 6 Steps to Solve Your Blood Sugar Problems Permanently
- Antibiotic Resistant Infections: The Dangers… and How You Can Avoid Them
- What Really Happens When You Take Antibiotics?
- Understanding Inflammation and How to Eliminate It Naturally
- Listen to Your Body. Correct Food Ratios. Reverse Disease.
- Cholesterol Myths Debunked
- Follow The Money In “Sick-Care”: What’s Behind The Drugs And Needles?
- What Happens In Your Body When You Suffer From Thyroid Disease?
About the author:
 Raluca Schachter is a dedicated Clinical Nutritionist / Natural Health Practitioner a.k.a “The Health Detective”. Raluca was able to naturally reverse chronic health conditions she was struggling with most of her life, and now uses her knowledge to help as many people as possible do the same. Her health programs and diet plans offer a very unique and comprehensive approach to health, where individual nutritional and biochemical requirements are firstly met using specific nutrients and foods that each metabolism thrives on. Raluca offers her services to international clientele and her practice is fully online based. You can connect with Raluca at www.metabolicenergy.net and https://www.facebook.com/raluca.schachter.metabolicenergy
Raluca Schachter is a dedicated Clinical Nutritionist / Natural Health Practitioner a.k.a “The Health Detective”. Raluca was able to naturally reverse chronic health conditions she was struggling with most of her life, and now uses her knowledge to help as many people as possible do the same. Her health programs and diet plans offer a very unique and comprehensive approach to health, where individual nutritional and biochemical requirements are firstly met using specific nutrients and foods that each metabolism thrives on. Raluca offers her services to international clientele and her practice is fully online based. You can connect with Raluca at www.metabolicenergy.net and https://www.facebook.com/raluca.schachter.metabolicenergy
[pro_ad_display_adzone id=”110027″]