 By Carol Vander Stoep, RDH, BSDH, OMT
By Carol Vander Stoep, RDH, BSDH, OMT
Guest Writer for Wake Up World
Originally published at mercola.com and reproduced here with permission.
Viper venom is an efficient killer. Its swirls of toxic proteins multitask. Some paralyze the nervous system of the victim by blocking nerve-to-muscle messages. Others can misdirect messenger hormones, dissolve tissues, or make blood so sticky the resulting clots stop the heart, or thin it to the point that the victim quickly bleeds out.
[pro_ad_display_adzone id=”110028″]
Just as surely, dead or dying human teeth can harbor similarly lethal agents working on at least as many levels throughout your body. The sophisticated multi-level attack of oral microbes, their metabolic waste products, and their interaction with dental materials can similarly give rise to an immune system crash, which can manifest in a multitude of disguises. Is a root canal procedure a gamble you really want to take?
Economics versus Health: There Is Always a Price
The complexity of interactions and time delay before oral toxins express noticeable symptoms, compared to fast-acting snake venom, work well for the institution of dentistry and dental insurance companies, but it does not bode well for you.
Institutions are by nature invested in the status quo. The insurance industry’s business model is no different from most other business models – it values their bottom line over your health. We are left on our own to tease out root causes of disease.
It is only after the scare of cancer, the exhaustion of chronic fatigue, a nervous system derailment causing Parkinson’s tremors, Multiple Sclerosis (MS), or Bell’s Palsy, or even autoimmune issues such as lupus or ALS (Lou Gehrig’s disease), that some people make the difficult decision to consider a “dental revision” to help their body recover.
A dental revision is no less than removing all possible toxic stressors of oral origin – dead teeth, dead jawbone, heavy metals like mercury, nickel, and chromium, gum disease therapy, and often, removing meridian blockers like implants.
A dental revision may seem like a drastic and expensive step, but what is the cost of poor health to which these contribute? You can escape to clean mountain air or the ocean’s cleansing waves, but you can never escape your internal environment.
The two lab reports in this file1 are but two examples of DNA sequenced microbial profiles found in the jawbone socket of an extracted root canal treated tooth, and in cavitations. The root canal treated tooth showed no clinical or physical signs of failing. These interesting lab reports also connect the pathogens with their waste products’ target tissues.
What Is a Root Canal?
A root canal is an embalming procedure dentists perform on a tooth. Root canals are designed to keep a dead tooth mechanically functioning in a live body.
Teeth die as a result of trauma (including sometimes, the trauma of a high speed drill creating too much heat or sucking the organic material from the microscopic tubules that assist in keeping it alive), or from microbial invasion from deep decay or gum disease into the pulp that nourishes each tooth. The following video offers key considerations about root canals.
It is no longer a huge secret that root canals crank out microbial metabolic toxins. Even some root canal specialists (endodontists) are starting to “own” it. For instance, they acknowledge that “condensing osteitis” around a root-canal treated tooth is common.
As the video above mentions, condensing osteitis is a thickening of the bone around a dead tooth as your body tries to wall off the infective toxins seeping from it. On the other hand, the American Association of Endodontists (AAE) position statement2 on the matter (2012) states that:
“…the practice of recommending the extraction of endodontically treated teeth for the prevention of NICO [painful jawbone death due to poor blood supply], or any other disease, is unethical and should be reported immediately to the appropriate state board of dentistry.”
And yet, according to a 2006 study published in the Journal of Evidence Based Dental Practice:3
“[A] recent evidence-based review of the outcomes of both treatment modalities noted that if evidence-based principles are applied to the data available for both treatment modalities, few implant or endodontic outcome studies can be classified as being high in the evidence hierarchy.”
Is a Root Canal Right for Your Situation?
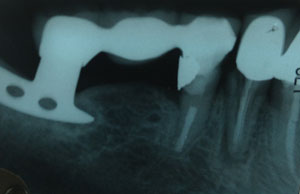
Image shows a root canal treated tooth anchoring one side of a bridge, an implant anchoring the other side |
No doubt about it, losing a tooth can be emotionally charged. I think it is one reason dentists work so hard to perfect tooth embalming procedures. The decision tree for considering tooth replacement is complex, and the solutions all involve compromise. There are a lot of hop off places for people to enter into De Nile.
Examine your own health status, priorities and philosophies and go with your best solution. “I have three root canals? What do I do now? Are all root canals toxic? “Probably. Eventually. Yet people have varying abilities to sustain the stress of toxins – and of course that ability varies over time.
Some biological doctors may recommend a root canal if a patient has a strong immune system, great genetics, and superior lifestyle. They suggest if one’s immune system crashes it can always be extracted later. But we are besieged by so many unavoidable immune system challenges in today’s world; I’m personally moving further and further away from the idea of assaulting my immune system with avoidable challenges.
Proper Diagnosis Is Key for Failing Root Canals and Cavitations
Since health effects of root canals and cavitations are similar, and one can arise from the other, I’ll digress to talk about cavitations for a moment. The existence of cavitations, also known as ischemic osteonecrosis (death of bone due to lack of adequate blood supply) when there is no pain present, and NICO when there is pain, seems to equate to a religious belief. Do cavitations exist or don’t they?
The preferred answer might depend on if you have skin in the game. Root canal specialists, state dental boards, and insurance companies cast aspersions on their existence, and (as noted above) even threaten to take away a dentist’s credentials should they acknowledge cavitations and recommend surgically treating the dead bone or extracting a root canal treated tooth to prevent them. Like the huge disservice of the domestic cooking oil manufacturers’ vilification of tropical fats decades ago, the stance of these special interests may equally hurt public health.
Part of the problem is that diagnosis is difficult. Typical dental x-rays can no more accurately diagnose cavitations than they can accurately diagnose subtle root canal pathology. They show only the most obvious cavitations. CT scans are excellent if all metals are absent from the mouth, but they are expensive and come with the added price tag of high radiation exposure.
There is no definitive way to judge how infected a root canal treated tooth or cavitation is, but a traditional camera-imaged thermogram, which many also use to detect early stage breast cancer, can offer some guidance. Thermographic images display infrared heat emissions, with each color gradation indicating different heat emissions. High-heat emissions are suggestive of inflammation, which may indicate root canal toxicity or a cavitation—even if you’re asymptomatic. You can read more about the use of thermography on PositiveHealth.com’s website.4
Regulation Thermometry
A new type of system, the AlfaSight™ 9000, offers a more comprehensive and precise thermograph than the more widely known digital-imaging camera thermography mentioned above. This more objective thermometry system delivers a functional physiologic assessment of your body’s bio-regulation system and offers insights into underlying dysfunction that both precedes and provokes developing disease processes.
Infrared measurements of skin temperature at over 100 points on your body including your head, torso, and back, taken both before and after exposure to a cool ambient room temperature assess how your body regulates temperature stress via the autonomic nervous system. Connected organs, glands, and other tissues influence the capillary blood vessel bed beneath each skin point location. Changes indicate either clear or blocked channels.
Scientific evidence shows that internal physiological abnormalities and dysfunction affect skin surface temperatures and that, therefore, skin temperatures and behavioral responses can reveal information about associated organ function. Medical clinics worldwide have studied, correlated, and validated over 40 temperature patterns that define regulation incapacities, called signature recognitions. Alfa Thermodiagnostics’ AlfaSight™ 9000 captures these signature patterns and provides a vivid integrative, computerized summary report5 that illustrates a system-wide overview and detailed dental, breast, and prostate evaluations.
Other Diagnostic Tools
Cavitat. Just as seismologists use acoustic energy to look for oil and obstetricians image fetuses with ultrasound, some dentists use a Cavitat to explore 3D images of cavitations in jawbone. As with first generation Thermography, it requires a skilled clinician and there is room for error. In the process of gaining FDA approval, tests using the Cavitat showed that 94 percent of old extraction sites were positive for bone lesions. Perhaps not surprisingly, Aetna Insurance discredited cavitations and the Cavitat. As Dr. Wes Shankland states in an open letter:
“Aetna Insurance Company contacted other insurance companies and reported that jaw bone cavitations did not exist. Aetna Insurance Company also informed others that the Cavitat was inaccurate and those who used this device were ‘quacks.'”
Such negative and inaccurate publicity literally ruined Cavitat sales. With no other recourse, Cavitat Medical Technologies made a decision to file a federal lawsuit, in Denver, against Aetna Insurance Company. Aetna lost and was ordered to pay a serious judgment, but the damage was done.
EAV (Electro Acupuncture according to Voll). An EKG measures electrical flow through your heart. Expressed as a graph, it pinpoints heart damage, since current does not flow through dead tissues. EAV works the same way. The EAV test uses an ohmmeter to measure energy flow along meridians at acupuncture points. If you understand meridians and you’ve signed on to “Healing is Voltage,” “The Body Electric” and understand the science behind “Earthing”, you know low-functioning organs are low in negative ions.
This state hinders electron flow along your body’s energy meridians. Dr. WA Tiller, Professor Emeritus of Materials Science at Stanford University, set out to discredit the EAV, but became an advocate as his research verified organ degeneration correlated with low conductance. In fact, it was Dr. Tiller who mapped the Meridian Tooth Chart,6 which correlates each tooth with its associated organs, glands, and anatomical structures on the same meridian. Infected or diseased teeth, as well as dental implants, block electrical conductivity on meridians and so can alter the health of other organs located on the same meridian and vice versa.
The Dark Side of Implants
Perhaps you have decided you must extract your root canal treated teeth to maintain or regain health—against the clear position stated by the American Association of Endodontists above. You chose a biological dentist who can help you avoid cavitations, and boosted your immune system. How should you replace the space? Interestingly, the more complex and biologically incompatible the option, the more costly it is. Costs vary widely, as do longevity estimates.

|
Implants are essentially an artificial root screwed into your jawbone, topped with an artificial tooth or used as an anchor for a bridge or partial denture. Implants are displacing root canals because they look, feel, and function very much like a natural tooth, and do not interfere with normal oral activities.
They help maintain bone that normally dissolves over time after a tooth is extracted. They can last a long time, and do not require grinding down adjacent teeth, as a fixed bridge would require. But you have to remember success is not measured only by tooth function, but function within your body as a whole.
Here are a few important aspects of dental implants you must seriously consider before making the decision to go forward with this major investment. Dead tissues do not conduct energy, implants therefore, whether titanium or zirconium, slow energy flow along meridians. Your body must constantly compensate for this. As with root canals, your associated organs, glands, or anatomical structures may functionally decline.
Most people with a dental implant have other metallic dental repairs present, which only exacerbates energetic chaos. In fact, the implant screw and replacement tooth are usually different metals. These two dissimilar metals within an electrolyte (saliva) effectively turn your mouth into a battery. Additionally, if you still have gold, mercury, copper, tin, silver filings, or nickel-based crowns in your mouth, these will also contribute to the galvanic currents being generated.
What You Need to Know About Titanium Implants
Most implants used today are made of titanium. So when your mouth is functioning as a battery due to the dissimilar metals present, there are resulting chaotic galvanic currents that continuously drive ions from the titanium or its alloys, which include small amounts of vanadium or aluminum. These metallic ions are then transported around your body, around the clock, where they bind to proteins and can wreak havoc with your health. Some people are more susceptible to the resulting inflammatory, allergy, and autoimmune problems than others. There is a blood test7 to help determine this sensitivity.
Though you’re exposed to fluoride through many avenues, tap drinking water and dental products remain your most significant sources. If you drink tap water or use fluoridated toothpaste, it is important to know that fluoride accelerates titanium corrosion in the extreme (up to 500 microg/(cm2 x d)). Low pH values (acidity in the mouth or a dry mouth) accelerate this effect profoundly.8 Of course, corrosion of the other metals also accelerates ion release.
Previous research9 has documented that:
“The amounts of tin released by the enhanced corrosion of amalgam [in the presence of titanium] might contribute measurably to the daily intake of this element; the corrosion current generated reached values known to cause taste sensations. If the buffer systems of adjacent tissues… are not able to cope with the high pH generated around the titanium, local tissue damage may ensue; this relationship is liable to be overlooked, as it leaves no evidence in the form of corrosion products.”
While most people do not notice galvanic currents, others experience unexplained nerve shocks, ulcerations, a salty or metallic taste or a burning sensation in their mouth. Noticeable or not, oral galvanic currents are commonly as high as 100 micro-amps, yet your brain operates on 7 to 9 nano-amps—a current more than 1,000 times weaker. Given your brain’s proximity to your mouth, biological dentists are concerned the constant high and chaotic electrical activity may misdirect brain impulses. These currents can contribute to insomnia, brain fog, ear-ringing, epilepsy, and dizziness.
The possibility that titanium implants may act as antennas that direct microwaves from your cell phone and cellular transmission towers into your body also deserves study. As Dr. Douglas Swartzendruber, a professor at the University of Colorado has said: “Anything implanted in bone will create an autoimmune response. The only difference is the length of time it takes.”
Titanium implants are certainly known to suppress important immune cells such as your T-cells, white blood cells critical to immune system function, and create oxidative stress as measured by rH2 values (a measurement of oxidation-reduction potential under a specific pH). Diseases associated with implants are not all that different from those associated with root canals, and include a number of different autoimmune and neurological disorders, such as:
| Cancer | Multiple sclerosis (MS) | Alzheimer’s disease |
| Parkinson’s disease | Chronic fatigue | Fibromyalgia |
Other complications of implanted titanium include occasional facial eczema as your skin tries to detoxify the titanium ions. Dental implants also have no fibrous “seal” to prevent microbial invasion. If you make the decision to get a dental implant, it’s wise to use floss impregnated with ozonated oil around the neck of each implant daily.
Alternatives to Titanium Implants
Zirconium implants are a newer innovation in dentistry and many biological dentists now use them. These implants bypass some of the problems of titanium mentioned above. They still block energy flow, but at least they are electrically neutral, eliminating the potential to interfere with your brain impulses. The implant itself also does not contribute to electrical galvanic currents being generated in your mouth. But you still need to be careful as the artificial tooth that is ultimately screwed onto the zirconium implant may have a metal base. Zirconium implants also release ions, but at a much slower rate than titanium implants.
These implants seem to last quite a long time. One systematic review showed that over the 10-30 year period studied, there was only a 1.3 percent to five percent loss of implanted teeth in clinically well-maintained mouths. For those with less optimal maintenance, it was more like a 14-20 percent loss of implanted teeth over that time. Don’t even think about smoking though! Endodontic literature has a very different slant on the benefits of implants, of course.
Traditional Bridges Can Be Costly and Relatively Impermanent
 First off, bridges don’t last all that long. The average bridge lasts eight years, with a range of five to 15 years. For this reason, “permanent bridges” are no longer considered “permanent.” A traditional bridge is comprised of several units – the artificial teeth and the abutments. Abutments are the crowns (caps) made to cover the anchor teeth. The bridge is permanently bonded in place to span a gap that replaces at least one missing tooth. Broken down or completely intact, the abutment teeth to each side of the gap are aggressively cut away to accept the covering crown.
First off, bridges don’t last all that long. The average bridge lasts eight years, with a range of five to 15 years. For this reason, “permanent bridges” are no longer considered “permanent.” A traditional bridge is comprised of several units – the artificial teeth and the abutments. Abutments are the crowns (caps) made to cover the anchor teeth. The bridge is permanently bonded in place to span a gap that replaces at least one missing tooth. Broken down or completely intact, the abutment teeth to each side of the gap are aggressively cut away to accept the covering crown.
Or should I say smothering crown? In my video above, I used an analogy of a healthy tooth being like a fountain. A crown stifles the natural nutritive, cleansing, hydrating flow of lymph. It can no longer “breathe.” Why do this to two good teeth that need no dental work for the sake of one (or two) missing teeth? Some biological doctors think these should be removed periodically so the underlying teeth can be cleaned up.
If one of the supporting crowned teeth breaks or develops decay or nerve damage, the bridge and its three or more crowns must be removed and replaced. As a hygienist, I can tell you that most people are terrible about cleaning around the abutment teeth and under the artificial tooth. Margins are very susceptible to decay. Again, I advise my clients to use ozonated oil around all crown margins as an extra degree of caution. Good personal care is one key to longevity. And once again, avoid smoking!
I am no fan of crowns as I explained in a previous interview with Dr. Mercola. The more a tooth is destroyed during restoration, the less able it is to withstand chewing forces. Also, forces which once could transfer through the organic, flexible bulk of the tooth to the root now must travel along the outside of a stiff crown to concentrate at the gum margin – hardly a recipe for longevity of either the underlying tooth or the crown itself.
Biomimetic Considerations to Take into Account
Biomimetic means mimicking nature. In choosing dental materials, a dentist must weigh the ability of the body’s immune system to ignore dental materials after recognition, called biocompatibility, with the beauty and function patients demand. They must find materials that match the flexibility of teeth so they can absorb daily chewing and clenching stresses. Materials should expand and contract at the same rate as teeth do when exposed to oral temperature fluctuations and they must resist wear and fracture.
Porcelain crowns are about four times harder than natural teeth and accelerate wear on opposing teeth. They fracture far more easily than zirconia based ceramic crowns, which are biocompatible, beautiful, and strong. These benefits come at the cost of stiffness. Zirconia based ceramic crowns are poor shock absorbers, which can be hard on your jaw joint and the bones that anchor your teeth. A new material, poly-ceramic DiamondCrown, comes closer to meeting all these requirements, and is biocompatible for about 80 percent of people tested. More biocompatible and biomimetic dental materials will emerge as these principals are more widely recognized.
Other Points to Consider
Your cranial (head) bones rhythmically move. Their gentle movements are thought to help drain your sinuses, aid nasal breathing, and influence your nervous system via movement of cerebrospinal fluid, the fluid that bathes your brain and nerves in your spinal cord.
This rhythmic pumping of cranial bones is particularly important at night because it helps the glymphatic system flush waste products from your brain that have built up during the day. Think of the glymphatic system as your brain’s garbage truck; glial cells create high pressure channels for cerebrospinal fluid that dilate and flow during sleep as blood pumps through arteries and as cranial bones “breathe.” They close during wakefulness. When movement is restricted, migraines or a build-up of the amyloid plaques associated with Alzheimers can occur. The glymphatic system may be one of the most important reasons you sleep.
TMJ (jaw joint) specialists, osteopaths and craniosacral therapists recognize the need to maintain cranial bone motion. These clinicians suggest that no fixed dentistry, whether “permanent” bridgework or metal partial, should cross the midline of the upper or lower jaw.
If you choose to have a permanent bridge, avoid porcelain fused to metal, since these metals contain nickel. Some dentists will assure you that they would never use a nickel-based metal; they use stainless steel! But stainless steel contains at least 10 percent chromium, vanadium, and nickel and/or manganese. I recommend going metal-free!
Fixed bridges were once considered premium care, since they, like implants, look, feel and function much like permanent teeth. In my experience, both require about the same amount of extra personal and clinical care. Incidentally, dentists will occasionally recommend a cantilever bridge, anchoring a false tooth to just one neighbor instead of two. These are less costly, but can certainly torque the anchor tooth, which it cannot always withstand.
Resin Bonded Bridge—A Less Costly Alternative, But Just as Impermanent
Resin bonded bridges (Maryland bridges) are a minimally invasive option for replacing missing teeth in certain situations. They are generally only considered for anterior tooth replacement. Design, materials, skill, and patient selection largely dictate longevity and satisfaction. Fortunately, design and materials have significantly evolved. Unlike traditional bridges, resin bonded bridges require much less reduction of supporting teeth. Instead, the dentist slightly reduces the backs of the neighboring teeth onto which “wings” attached to the artificial tooth are bonded.
Materials can be all resin, porcelain, porcelain bonded to metal, or zirconium. Most doctors still fabricate these bridges with a wing to either side of the artificial tooth, though the literature seems to suggest it is better to just have one – to cantilever the missing tooth off one supporting tooth. Interestingly, this is because it is recognized that cranial bones and teeth move and that the anchoring teeth do not move equally. This puts stress on the bonds, which can lead to failure. Also, since it is unlikely that both bonds would break at the same time, the debonding often goes unnoticed, allowing decay to set in under the debonded wing.
Resin bonded bridges are a good option for adolescents with missing teeth, when the bridge is well designed. Most replacement options cannot be considered until you have finished maturing physically. These bridges help maintain space and are fairly easy to care for.
If you have teeth that have loosened due to gum disease, some would add another advantage of resin bonded bridges – they help splint loosened teeth together. This is true, but unless your gums are disease-free and cleaned on a daily basis at home, it might be time to remove them because in this case, it might be extremely difficult to self-cleanse daily at home. We are not just looking at longevity of the teeth, but longevity of the host.
The downside of resin bonded bridges is that they’re somewhat fragile. If made with metals, the usual caveats apply: mixed metals lead to galvanic currents and a panoply of problems already addressed. Again, 100 percent zirconium would avoid this. Remember, biological dentists try to be metal free and avoid metal-based crowns and bridges. It isn’t just the galvanic currents these set up, but the release of nickel/chromium/manganese/vanadium ions. A better restoration option might be the Carlson Bridge – a resin bonded bridge that requires no drilling into adjacent teeth. Placed in one appointment, these economical, prefabricated, “winged” replacement teeth can last many years. An advantage is that the bond to adjacent teeth is less rigid, so cranial bones can shift as they should.

Partials—Your Least Expensive Option
Going back in time, removable partials were all dentistry offered to replace missing teeth. Our current culture values looking young, so partials – associated with our grandparents – are a difficult aesthetic choice. They may however be the choice that offers the best chance for aging well. Partials are designed based on how many teeth need replacing. Metal frameworks were once the norm, but the future lies in non-metal dental repairs. New materials:
- Are less obvious
- Avoid the adverse properties of metal restorations already discussed
- Are able to distribute chewing forces over a greater area compared to metal framework partials, and are therefore more comfortable
- Relines are less frequent
- According to the Clifford Biocompatibility Test, Flexite and Valplast (light, flexible, yet strong nylon resins) are biocompatible for 99 percent of the population. Lucitone FRS is a very similar biocompatible nylon resin. None of these use a heavy metal (cadmium) as a pink colorant as some other dental materials do. Many patients choose a clear framework to avoid any possible reaction to the colorant. Nylon materials can draw in water and with it, odors and stain, though good hygiene can mitigate this problem.
- VisiClear is another nylon-free biocompatible partial material

|
| The intentional exposed palate design in this partial means the wearer can continue good oral posture, which means properly keep the tongue in contact with the palate |
For best aesthetics, biocompatibility, and biomimetic function, choose DiamondCrown or zirconia teeth in your partial rather than the default acrylic teeth most often used. If you must add another tooth to any of the above partials, that is possible, too. The lab simply reuses the artificial teeth, the most valuable component, and remakes the framework with the new tooth!
Biocomp Labs10 and the Clifford Consulting and Research Lab11 offer individualized dental materials testing, recommended especially for those with multiple chemical sensitivities or anyone who needs dental work and feels their health could be challenged by the wide range of dental materials available.
Most patients tell me they consider these newer partials to be comfortable and aesthetically unnoticeable, though they are annoyed that foods tend to trap under them. People with spider partials tell me they often take them out to eat, but wear them the rest of the time to maintain the space until dentistry offers them more biocompatible “fixed” choices.
At least one reader will likely comment that if only people adopted a certain lifestyle, these kinds of advanced dentistry would be unnecessary. I couldn’t agree more.
The reality is that most people’s mouths are in deplorable shape. I try not to spend much time thinking about the rescue dentistry presented here. Most of my advocacy work centers around changing how we approach dentistry so your children or their children can avoid these compromising options.
Ultimately, the answers to better oral and general health start in infancy and include a radically different model of dentistry and definition of health. The answers are out there now (see Mouth Matters book and website12) along with a few clinicians who are well versed in these strategies. Seek them out, and if you can’t find someone who does the kind of dentistry you want in your area, be ready to ask them to learn it.
Resources to Help You Find a Biological Dentist
If you are seriously considering any of the dental procedures done above, it is best to have them performed by a biological dentist. The following organizations can help you to find a mercury-free, biological dentist that would best serve your needs:
- Consumers for Dental Choice
- International Academy of Biological Dentistry & Medicine (IABDM)
- Dental Amalgam Mercury Solutions (DAMS) – E-mail them at: [email protected]or call 651-644-4572 for an information packet
- Huggins Applied Healing – You’ll need to fill out a form and they will connect with you to find a suitable dentist in your area
- Holistic Dental Association
- International Association of Mercury Safe Dentists
Article sources:
- 1 Mouthmatters.com, Cavitations (PDF)
- 2 American Association of Endodontists Position Statement (PDF)
- 3 J Evid Based Dent Pract. 2006;6:101-109
- 4 Positivehealth.com, Thermography in Dental Practice
- 5 Alfa Thermodiagnostics, Thermometry-The AlfaSight 9000™ has obtained CE marking & Health Canada licensing & is on fast track for US FDA 510k clearance
- 6 Talkinternational.com, Meridian Tooth Chart
- 7 Melisa.org
- 8 Biomaterials. 1998 Aug;19(16):1495-9
- 9 Scand J Dent Res (1988 Oct) 96(5):466-72
- 10 Biocomp Laboratories
- 11 Clifford Consulting and Research
- 12 Mouthmatters.com
About the author:
Carol Vander Stoep, RDH, BSDH, OMT, is an advocate for change in dentistry. She believes mid-level providers – dental hygienists with expanded training – must be empowered to go beyond their serious limitations in the United States. Training a core of motivated hygienists at a clinic in Belize, her intent is to help bring an advanced model of Minimally Invasive Preventive Dentistry and posture-guided early facial development to India and China based on the model of “Barefoot Doctors.” A clinical hygienist, orofacial myofunctional therapist, lecturer, and writer, she brought many of these concepts together in her book “Mouth Matters: How Your Mouth Ages Your Body and What YOU Can do About It.”
[pro_ad_display_adzone id=”110027″]








