3rd September 2015
By Rajgopal Nidamboor Ph.D
Guest Writer for Wake Up World
A revolutionary, life-changing new surgical technique offers women with ‘absent vagina’ syndrome, or MRKH, the functional wherewithal to shed the dismal tag of stigma and misery, and embrace ‘born-again’ womanhood.
The Vagina Epilogue
First, a small story about an Indian gynaecologist who fell in love with a fellow doctor abroad. He knew that the lady he loved had a vital organ missing in her anatomy. Her vagina. The biological absence of the vagina — the Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome in medical phraseology — is a condition that occurs in 1 out of every 4,500 female births, which means it’s not exactly a rare condition, but is shrouded under a cloak of shame and secrecy. We all are aware too of how women without reproductive organs have been treated in our society down the ages. But the couple happened to read about a new revolutionary restorative surgical procedure in a medical journal that was being performed by a doctor in Mumbai, India.
[pro_ad_display_adzone id=”110028″]
They immediately sought an appointment with that doctor and headed home. The lady underwent the procedure successfully and got married to her love a few weeks later. It did not take long, thereafter, for the duo to find a surrogate mother who subsequently delivered their baby, something they could not have visualised even as a remote possibility just a few months previously.
Not every woman has this sort of a happily ever after, though. For a girl “cursed” with this congenital condition, it is nothing short of a death sentence. The eerie, empty syndrome not only impacts one’s emotional and psychological bearings, it also leads to ostracisation within the family’s immediate or outside circle, with the girl being labelled as barren and, therefore, a bad omen. All this happens because, as mentioned earlier, not much is known about this condition as it is not something that is even talked about, leave alone treated.
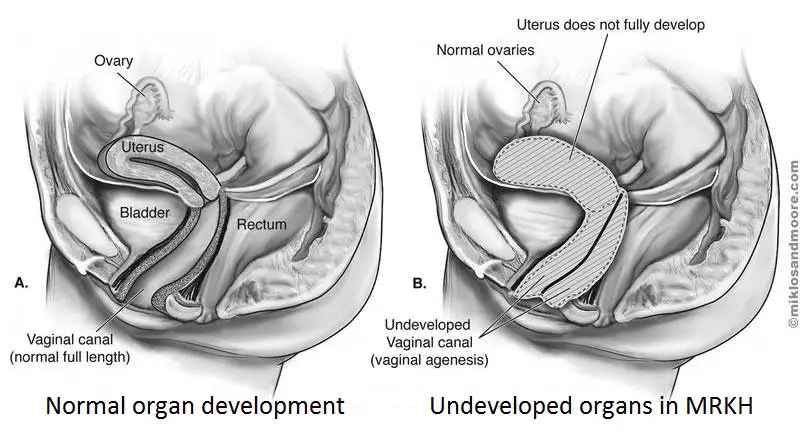
So, what exactly is MRKH? The development of the Müllerian duct is one of the ill-understood topics in gynaecology, although it forms the fundamental underpinning of every woman’s reproductive anatomy. The Müllerian ducts — named after Johannes Peter Müller, a German physiologist, who first described them — originate in the embryo. They culminate in what is called the Müllerian eminence in the primitive urogenital sinus (cavity). They also form the fallopian tubes, uterus and the upper portion of the vagina. The whole process is a marvel. Of how different segments of the Müllerian ducts develop into different structures — the fallopian tube as the thin supple peristaltic organ, the thick distensible and contractile uterus endowed with local immune function, the thick competent and distensible cervix and, of course, the extremely elastic vagina.
It is, indeed, nature’s amazing complexity that endows each part with diverse reproductive functions. The development and differentiation of the Müllerian ducts are not only important at the foetal stage, their progression in adult life explicates the pathogenesis of several gynaecological conditions, such as endometriosis — a disorder in which the tissue that normally grows inside the uterus extends outside of the uterus — and, ovarian neoplasm, or benign or malignant cancer.
To cut a long story short — the total absence of the Müllerian progression leads to aplasia, or defective development or congenital absence of the vaginal organ, while partial development, a common occurrence, leads to tubal and skewed uterine development, not to speak of the complete absence of the upper three-fourth of the vagina. In most cases of absent vagina, the uterus is typically incomplete, or rudimentary. The ovaries are, however, normal, but they are placed on the lateral pelvic wall, along with the uterus. The overall inference: a dire, barren prospect of being unable to conceive, or give birth to a child.
Most girls afflicted with this disorder may have normal secondary sexual development, such as the breasts. Yet, there may be associated congenital anomalies of the urinary tract — such as a horseshoe shaped kidney with the failure of the organ to develop during embryonic growth. This may be present in 30-40 per cent of individuals having MRKH syndrome, while 10-15 per cent may show skeletal anomalies.
 Is there a way for girls with the rudimentary vagina to have a normal, happy conjugal life? There is, thanks to revolutionary research and techniques formulated by doctors in the past and most recently by Dr Pravin Mhatre, a Mumbai-based gynaecologist, who also pioneered the world’s first avant-garde ovarian transplant, over a decade ago, along with Dr Jyoti Mhatre — a husband-wife team — and, Dr Rakhi Sahu. The novel procedure has earned plaudits from doctors and researchers alike, especially abroad. However, their work is yet to receive adequate attention in the country of its origin.
Is there a way for girls with the rudimentary vagina to have a normal, happy conjugal life? There is, thanks to revolutionary research and techniques formulated by doctors in the past and most recently by Dr Pravin Mhatre, a Mumbai-based gynaecologist, who also pioneered the world’s first avant-garde ovarian transplant, over a decade ago, along with Dr Jyoti Mhatre — a husband-wife team — and, Dr Rakhi Sahu. The novel procedure has earned plaudits from doctors and researchers alike, especially abroad. However, their work is yet to receive adequate attention in the country of its origin.
The Mhatre assay is a technological advance over several operative options available for the creation of ‘neovagina.’ It is practically free of complications and disadvantages of procedures in use, such as free skin graft, intestinal or sigmoid vaginoplasty, amnion graft, and pelvic peritoneum graft, not to speak of complications reported with varying patterns — viz., stenosis (narrowing), poor lubrication, scarring, dyspareunia (painful coitus) and the need for laparotomy, a surgical procedure, to overcome such negative barriers. Yet another downside of the ‘older’ procedures is the possibility of squamous cell carcinoma (cancer) from free skin graft and adenocarcinoma, a type of cancer that forms in the mucous-secreting glands of the body. This is not all. The amnion graft, or membrane transplantation, to ‘sculpt’ the neovagina, or vaginal ‘reconstruction,’ is suggested to transmit hepatitis, or human immunodeficiency virus (HIV), although the use of freeze-dried amnion has been evidenced to prevent such transmission.
Interestingly, the creation of neovagina by way of endoscopic-assistance (Vecchietti technique), in the recent past, has received much attention, yet the fact is the procedure is complex, time-consuming and laden with potential complications. The use of peritoneum — the serous membrane that forms the lining of the abdominal cavity — in vaginoplasty, a reconstructive plastic surgery and cosmetic procedure for the vaginal canal, was first popularised by Davydov, a Russian gynaecologist. He reported a series of 28 patients with good results in eight months. His conventional surgery is currently being replaced by laparoscopy, which was inevitable and also predictable. The laparoscopic modification has resulted in a shorter operating time and reduced post-operative morbidity. Yet, it does not have the advantages of the Mhatre technique.
This is not all. While several reconstructive surgical procedures have been described for vaginal agenesis, or failure of the vagina to develop, almost all of them are surgically challenging, multi-staged, time-consuming and have the likelihood of causing permanent scars on the abdomen, or the skin retrieval (graft) sites used for the reconstructive procedure.
The new simple and effective technique using laparoscopic peritoneal ‘pull-through’ for the creation of the neovagina is what the Mhatre duo and Sahu have pioneered and used with good, replicable results.
Their work also validates the procedure’s success in 36 patients, aged between 16 and 27. The trio used three different techniques for peritoneal vaginoplasty. They followed up on their patients for over a period of 1-7 years. The results are tangible — the peritoneal lining changes not only resembles normal vagina, but also provides for “excellent normal vaginal function.” More importantly, as the ovary became accessible via vagina, three patients underwent ovum retrieval and pregnancy, while using surrogate mothers, giving the whole process a life-changing tag — a fertility-enhancing procedure.
Interestingly, three of the patients were from the medical fraternity with two of them (read example two, relating to one of them, at the beginning of this piece) being gynaecologists.
Apart from routine pre-operative work-up, a diagnostic laparoscopy was performed to determine mobilisation and feasibility of creating anterior and posterior flaps for the peritoneal ‘pull-through’ to see the size and position of the utricles on lateral pelvic walls and also establishing the possibility of uterine implantation in the neovagina procedure.
During follow-up, as the Mhatres explain, the neovaginal space is dilated gradually to maintain the desired length till sexual activity is resumed. Dilatation using a glass dilator increases the length and diameter of the neovagina and also changes the axis ideal for intercourse. The neovagina, as the Mhatres put it, is in the precise anatomical axis. They also add that the pelvic peritoneum lining the neovagina is receptive to oestrogen, the female hormone.
The design of their study, as the Mhatres explain, was retrospective. As many as 90 per cent of patients required supervised glass dilatation in the first post-surgical week; 100 per cent of women required vaginal lubrication for the first three months. The need for lubrication declined drastically after 6-9 months in the married group of patients (66.5 per cent). While 50 per cent of patients complained of pain and discomfort in the first few weeks, pain-free intercourse followed after 3-6 months.
When the patients were asked their view on the optimal timing of surgery, 72 per cent favoured that the “operation should be performed earlier.” They contended that whatever delay that elapsed for seeking professional medical help was primarily because of the social disgrace attached to the absent vagina — aside from the general belief of correlation with the ‘transgender’ label, or some curse, or bad omen.
The results were impressive: the average operative time was 1-1.5 hours and the average hospital stay was three days, except in two cases, which required five days. There were no major complications, except for one patient who had a rectal problem. This was managed by suturing; the recovery was uneventful. On follow-up, the patients had adequate, comfortable vaginal length of about 7-8 cm, admitting full-size speculum. Sexual satisfaction on follow-up was also good. Of the 36 patients, nine were married and 15 patients got married after vaginoplasty. They reported of no sexual difficulty with themselves, or their partner. More than 90 per cent of patients were positively happy after having a successful vaginoplasty, with no obvious signs of surgery. The successful vaginoplasty (neovagina) procedure has not only reassured patients, with the incomplete ‘V,’ but it has also changed their and their families’ outlook and acceptance dramatically too.
If this isn’t a life-changing, medical perestroika for hapless girls, and women, with ‘absent’ vagina, to shedding the dismal shadow of misery, or stigma, and embracing ‘born-again’ womanhood, what is?
This article was first published in Financial Chronicle, India. © Financial Chronicle. Reproduced with permission.
Previous articles by Rajgopal Nidamboor:
About the author:
 Rajgopal Nidamboor is a board-certified wellness physician, fellow of the College of Chest Physicians (FCCP), member of the Center of Applied Medicine (M-CAM), writer-editor, commentator, critic, columnist, author, and publisher. His special interests include natural health and wellness, mind-body/integrative medicine, nutritional medicine, psychology, philosophy, and spirituality. His focus areas also encompass contemporary research and dissemination of dependable information for all people concerned about their health.
Rajgopal Nidamboor is a board-certified wellness physician, fellow of the College of Chest Physicians (FCCP), member of the Center of Applied Medicine (M-CAM), writer-editor, commentator, critic, columnist, author, and publisher. His special interests include natural health and wellness, mind-body/integrative medicine, nutritional medicine, psychology, philosophy, and spirituality. His focus areas also encompass contemporary research and dissemination of dependable information for all people concerned about their health.
Rajgopal feels that it is increasingly gratifying to see most people, including physicians, thinking outside the box – especially in areas such as natural health, where the body knows best to heal itself from the inside out. His published work includes hundreds of newspaper, magazine, web articles, four books on natural health, two coffee-table books, a handful of e-books, and a primer on therapeutics. He lives in Navi Mumbai, India.
Connect with Rajgopal Nidamboor at: health-prism.com
[pro_ad_display_adzone id=”110027″]