Contributing writer for Wake Up World
For the past four decades, the U.S. government has warned that eating cholesterol-rich foods such as eggs would raise your LDL cholesterol (inappropriately referred to as “bad” cholesterol) and promote heart disease. However, decades worth of research utterly failed to demonstrate this correlation, and the 2015-2020 Dietary Guidelines for Americans [1],[2],[3],[4],[5] finally addressed this scientific shortcoming, announcing “cholesterol is not considered a nutrient of concern for overconsumption.” [6]
This is good news, since dietary cholesterol plays an important role in brain health and memory formation, and is indispensable for the building of cells and the production of stress and sex hormones, as well as vitamin D. (When sunlight strikes your bare skin, the cholesterol in your skin is converted into vitamin D.)
Unfortunately, the dietary guidelines still cling to outdated misinformation about saturated fat, wrongly accusing it of raising LDL and contributing to heart disease. Here, science has shown that saturated fat only raises the safe, fluffy LDL particles. It also increases HDL, which is beneficial for your heart.
[pro_ad_display_adzone id=”110028″]
The guidelines became and are still confusing because the basic premise was wrong. Dietary fat is indeed associated with heart disease, but it’s the processed vegetable oils, which are loaded with trans fats and oxidized omega-6 fats, that are the problem, not saturated fats.
The introduction of industrialized, highly processed and frequently heated omega-6 vegetable oils distorted the vitally important omega 6-to-3 ratio, causing metabolic catastrophes. The problem was further exacerbated by replacing saturated fat with refined carbohydrates, which were incorrectly viewed as a healthier option, thanks to misinformation created and spread by the sugar industry.
Impairs Electrical Storage Potential of Your Cells
Nutrition and biochemistry are clearly important to your health, but so is your body’s electrical system. All our membranes are made of fats that are insulators and connected through a conductor. This arrangement sets up a biological capacitor to store electrons — but only if the fats are healthy.
If you consume damaged fats, or worse, heated and hydrogenated oils, the fatty acids in the cell membrane essentially become nonfunctional and unable to store body voltage, thus increasing the risk for disease. This is one of many reasons why it is so vital to eat healthy fats.
Unpublished Research Undermines Decades of Dietary Advice
Ancel Keys was one of the most prominent nutritional researchers of the mid-20th century. He gained enormous professional and influential prominence and his views were widely adopted by professional and public health organizations. His research formed the foundation for all of the low-fat recommendations that followed. Interestingly, some of his own follow-up research actually undermined his hypotheses on cholesterol and saturated fat, but these findings were never published.
Had they been, the cholesterol and low-fat myths might never have gained the same kind of traction. The four-decades-old study in question was unearthed by Dr. Christopher E. Ramsden, who specializes in digging up and reevaluating lost studies that challenge mainstream health advice.[7],[8],[9],[10],[11],[12],[13],[14],[15],[16]
Keys, who was largely funded by the sugar industry, is believed to have been responsible for suppressing this damning study, as it doesn’t support his original hypothesis. Only parts of the trial’s results were ever published, leaving out the controversial finding that replacing saturated fats with vegetable oil had no benefit on mortality. As reported by Scientific American:[17]
“Ramsden, of the National Institutes of Health, unearthed raw data from a 40-year-old study, which challenges the dogma that eating vegetable fats instead of animal fats is good for the heart. The study, the largest gold-standard experiment testing that idea, found the opposite …
Although the study is more than just another entry in the long-running nutrition wars — it is more rigorous than the vast majority of research on the topic — Ramsden makes no claims that it settles the question. Instead, he said, his discovery and analysis of long-lost data underline how the failure to publish the results of clinical trials can undermine truth.”
Saturated Fat Vindicated in Largest Most Rigorous Trial of Its Kind
Conducted from 1968 to 1973, the study [18] included 9,423 participants between the ages of 20 and 97, making it the largest trial of its kind. The participants were also residents of state mental hospitals and a nursing home, making it one of the most rigorously detailed studies as the meals of every person were carefully logged.
On the average, each patient was followed for about 15 months. Participants were randomly assigned to one of two groups, receiving either:
- A then-standard diet containing 18.5 percent saturated fat from animal fats such as milk, cheese, beef and shortening, and 5 percent unsaturated fat, based on total calories
- A diet in which 50 percent of the saturated fats were replaced with vegetable oil (a mainstay in today’s processed foods) and corn oil margarine (total 9 percent saturated fat and 13 percent unsaturated fat)
After analyzing the data, Ramsden and his team found that vegetable oils lowered total cholesterol levels by an average of 14 percent after one year. However, this lower cholesterol did not result in improved health and longevity, which is the conventional belief. Instead, the research showed that the lower the cholesterol, the higher the risk of dying!
For every 30 point drop in total cholesterol there was a 22 percent increased chance of death. In the 65 and older category, those who received vegetable oil experienced roughly 15 percent more deaths compared to seniors in the saturated fat group. The vegetable oil also did not result in fewer cases of atherosclerosis or heart attacks.
On the contrary, autopsies revealed both groups had similar levels of arterial plaque, but 41 percent of the vegetable oil group showed signs of at least one heart attack compared to just 22 percent of those in the saturated fat group. According to the authors:
“Available evidence from randomized controlled trials shows that replacement of saturated fat in the diet with linoleic acid [vegetable oil] effectively lowers serum cholesterol but does not support the hypothesis that this translates to a lower risk of death from coronary heart disease or all causes.”
Why Vegetable Oils Are so Bad for Your Health
Later this year I will post my interview with Dr. Cate Shanahan, author of “Deep Nutrition: Why Your Genes Need Traditional Food“[19], in which she delves into the profound harms done by processed vegetable oils in the modern diet. To learn more, keep your eyes open for that interview.
According to Shanahan, vegetable oil is your brain’s worst enemy, attacking it “at seven distinct vulnerability points using seven distinct strategies. All seven strategies are at work in causing autism and other childhood neurologic disorders.” This includes:
- Promoting gut inflammation and leaky gut. This inflammation often causes heartburn, which can serve as a red flag. Unfortunately, many misattribute heartburn to spicy foods rather than the more significant culprit, namely vegetable oils
- Disrupting the regulation of blood flow through the arteries in your brain and depleting your brain of antioxidants
- Turning your immune system against you by affecting your white blood cells (immune system cells), causing disease and nerve degenerating reactions
- Attacking the nerve cellular architecture. “Vegetable oils cause an overload of oxidative reactions inside the cell, leading to the accumulation of intracellular trash. When this affects our white matter, we lose our mobility. When it affects our gray matter, we lose our personalities and our connections to the world,” Shanahan explains in her book.[20]
- Impairing brain development through mutagenic effects on DNA and altered epigenetic expression
Other reasons why vegetable oils cause heart disease and other health problems include the following:
- Omega-6 polyunsaturated fats, when taken in large amounts, cannot be burned for fuel. Instead, they’re incorporated into your cellular and mitochondrial membranes, where they are highly susceptible to oxidative damage. As a result, your metabolic machinery is damaged. Vegetable oils made from genetically engineered (GE) crops (as most are) have additional health risks, as they tend to be loaded with toxic herbicide residues like Roundup.
- While your body needs some omega-6, most get far too much of it compared to omega-3, and this lopsided ratio can also have adverse health consequences.
- When heated, vegetable oils tend to oxidize. According to Dr. Fred Kummerow,[21] who has researched lipids and heart disease for eight decades, oxidized cholesterol is the real culprit that causes heart disease. By triggering inflammation, it promotes the clogging of arteries and associated cardiovascular problems, including heart attacks.
Many Studies Have Debunked the Saturated Fat Myth
Several other studies have also demonstrated that replacing saturated fats with vegetable oils is a bad idea. While the benefits for cardiovascular mortality and risk-factor reduction have been mixed, none of these trials showed that restricting saturated fats reduced total mortality:
|
Recovered data from the Sydney Diet Heart Study: In 2013, Ramsden’s team analyzed four trials looking at the effects of replacing saturated fats with vegetable oils. Replacing saturated fats with linoleic acid-rich vegetable oils increased mortality risk from all causes, including coronary heart disease and cardiovascular disease.[22] |
| The Oslo Study (1968): A study of 412 men, aged 30-64 years, found eating a diet low in saturated fats and high in polyunsaturated fats had no influence on rates of sudden death.[23] |
| L.A. Veterans Study (1969): A study of 850 elderly men that lasted for six years is widely used to support the diet-heart hypothesis. No significant difference was found in rates of sudden death or heart attack among men eating a mostly animal-foods diet and those eating a high-vegetable oil diet. However, more non-cardiac deaths, including from cancer, were seen in the vegetable oil group.[24] |
| London Soybean Oil Trial (1968): This study of nearly 400 men that lasted for two to seven years found no difference in heart attack rate between men following a diet low in saturated fats and high in soybean oil and those following an ordinary diet.[25] |
| The U.S. Multiple Risk Factor Intervention Trial (MRFIT): Sponsored by the National Heart, Lung and Blood Institute, this is another study that is highly misleading. It compared mortality rates and eating habits of over 12,000 men, and the finding that was widely publicized was that people who ate a low saturated fat and low-cholesterol diet had a marginal reduction in coronary heart disease. However, their mortality from all causes was actually higher.[26] |
|
A 2013 editorial published in the BMJ described how the avoidance of saturated fat actually promotes poor health in a number of ways. As stated by the author, Dr. Aseem Malhotra, an interventional cardiology specialist registrar at Croydon University Hospital in London:[27] “The mantra that saturated fat must be removed to reduce the risk of cardiovascular disease has dominated dietary advice and guidelines for almost four decades. Yet scientific evidence shows that this advice has, paradoxically, increased our cardiovascular risk … The aspect of dietary saturated fat that is believed to have the greatest influence on cardiovascular risk is elevated concentrations of low density lipoprotein (LDL) cholesterol. Yet the reduction in LDL cholesterol from reducing saturated fat intake seems to be specific to large, buoyant (type A) LDL particles, when in fact it is the small, dense (type B) particles (responsive to carbohydrate intake) that are implicated in cardiovascular disease. Indeed, recent prospective cohort studies have not supported any significant association between saturated fat intake and cardiovascular risk. Instead, saturated fat has been found to be protective.” |
|
A 2014 meta-analysis published in the Annals of Internal Medicine (which included data from 76 studies and more than a half-million people) found that those who consume higher amounts of saturated fat have no more heart disease than those who consume less. Moreover, those who ate higher amounts of unsaturated fat, including both (healthy) olive oil and (unhealthy) corn oil — both of which are recommended over saturated fats — did not have lower incidence of heart disease.[28] |
|
A 2015 meta-analysis published in the BMJ also failed to find an association between high levels of saturated fat in the diet and heart disease. Nor did they find an association between saturated fat consumption and other life-threatening diseases like stroke or type 2 diabetes.[29] |
In summary, industrially processed, highly refined vegetable oils do not reduce your risk of dying from heart disease. Put another way, saturated fats do not increase your risk of dying from heart disease either. Moreover, reducing cholesterol is not necessarily a sign of improved health; it may actually increase your risk of death. As noted by Ramsden:[30]
“One would expect that the more you lowered cholesterol, the better the outcome. But in this case the opposite association was found. The greater degree of cholesterol-lowering was associated with a higher, rather than a lower, risk of death.”
Statins Revisited
The cholesterol myth has been a boon to the pharmaceutical industry, as cholesterol-lowering statins — often prescribed as a primary prevention against heart attack and stroke related to high cholesterol — have become one of the most frequently used drugs on the market. In 2012, nearly 28 percent of American adults over the age of 40 reported using a statin.[31]
Updated cholesterol treatment guidelines issued by the American College of Cardiology and the American Heart Association (AHA) in 2013 made another 9.3 million Americans eligible candidates for the drug. However, researchers have repeatedly warned the cardiovascular risk calculator[32] used may be overestimating your risk by anywhere from 75 to 150 percent.[33] This means even healthy people at low risk for heart problems are being turned to statins.
What’s worse, the guideline also removed the recommendation to use the lowest drug dose possible. Instead, the sole focus is on statin-only treatment at higher dosages. The guidelines also ignore the density of the lipoproteins (the LDL and HDL). Large fluffy LDL particles are not harmful. Only small dense LDL particles can potentially cause problems as they can squeeze through the lining of your arteries. If they oxidize, they can cause damage and inflammation.
This means you could potentially have an LDL level of 190 but still be at low risk as long as your LDLs are large, and your HDL-to-total cholesterol ratio is above 24 percent. As mentioned earlier, saturated fat not only increases your HDL, it also increases large, fluffy LDLs, which is what you want.
[pro_ad_display_adzone id=”110030″]
Two Leading Cholesterol Guidelines Differ in Their Recommendations
Now, researchers have revisited the cholesterol guidelines, noting there are significant differences between the two leading guidelines in the U.S.[34] In 2016, the U.S. Preventive Services Task Force (USPSTF) released its own cholesterol treatment guidelines, which suggests statins should not be used unless the patient has at least one other risk factor (such as high blood pressure, diabetes or smoking) in addition to having a 10 percent risk on the cardiovascular risk calculator.
Under these guidelines, an estimated 17.1 million Americans are candidates for a statin, compared to the 26.4 million covered by the American College of Cardiology/AHA guidelines. The differences between the two guidelines have caused a great deal of debate among experts.
Which one’s better? As Michael Pencina, a professor of biostatistics and bioinformatics at the Duke Clinical Research Institute and lead author of the study told CNN:[35] “There’s generally confusion on who should be getting statins. I don’t think we have the perfect guideline yet.”
In my view, the number needed to treat offers compelling clues to the overall uselessness of statins. According to an analysis by the USPSTF, published last year:[36]
- 100 people need to take a statin as a primary preventive for five years in order for one or two people to avoid a heart attack, and none will actually live longer
- 250 people need to take a statin for up to six years in order to prevent a single death from any cause
A 2015 report[37] published in the Expert Review of Clinical Pharmacology concluded that “statistical deception created the appearance that statins are safe and effective in primary and secondary prevention of cardiovascular disease.”
By using relative risk reduction, the trivial benefits of statins are amplified. If you look at absolute risk, statin drugs benefit a mere 1 percent of the population. As noted by the USPSTF, this report found that out of 100 people treated with the drugs, one person will have one less heart attack.
Statins Do Not Reduce Mortality, and Can Seriously Harm Your Health
Other studies[38] have also found that statins provide no reduction in mortality when used preventatively — even in at-risk groups. This strongly suggests statins have even less of a benefit among those already at low risk of heart disease. Recent research[39] has also confirmed that high cholesterol is not linked with heart disease in the elderly, prompting the researchers to conclude that reducing cholesterol levels with statin drugs is “a waste of time.”
Indeed, Stephanie Seneff, Ph.D. and senior scientist at MIT, believes heart disease is a cholesterol deficiency problem, which is essentially the converse of the conventional paradigm. Still, her hypothesis appears to be supported by studies showing people with higher levels of cholesterol actually live longer than those with lower levels.
Aside from being a “waste of time” and not doing anything to reduce mortality, statins also carry with them a list of over 200 side effects and clinical challenges, including:[40],[41]
| Increased risk of diabetes (there are several mechanisms for this, including increasing insulin resistance and raising your blood sugar). | Acute liver disease. | Muscle pain, tenderness or weakness. |
| Rhabdomyolysis (a condition involving the death of muscle fibers). | Acute kidney failure. | Chronic liver dysfunction. |
| Reduced ketone production.[42] Ketones are water-soluble fat nutrients important for tissue health.
They’re also important molecular signaling molecules. |
Depletes your body of essential vitamins, minerals and nutrients, including CoQ10 and vitamin K2, both of which are important for cardiovascular and heart health. | Impaired fertility and reduced sex drive.
Importantly, statins are a Category X medication, meaning they cause serious birth defects, so they should NEVER be used by a pregnant woman or women planning a pregnancy. |
| Increased risk of cancer. Long-term statin use (10 years or longer) more than doubles women’s risk of two major types of breast cancer: invasive ductal carcinoma and invasive lobular carcinoma.[43] | Nerve damage. Research has shown statin treatment lasting longer than two years causes “definite damage to peripheral nerves”.[44] | Reduced muscle and nervous system coordination . |
| Diarrhea and/or constipation. | Dizziness. | Headache. |
| Central nervous system toxicity. | Abdominal pain. | Cataracts. |
| Decreased heart function.[45] | Endocrine dysfunction. | Memory loss. |
Making Sense of Your Cholesterol Levels and Assessing Your Heart Disease Risk
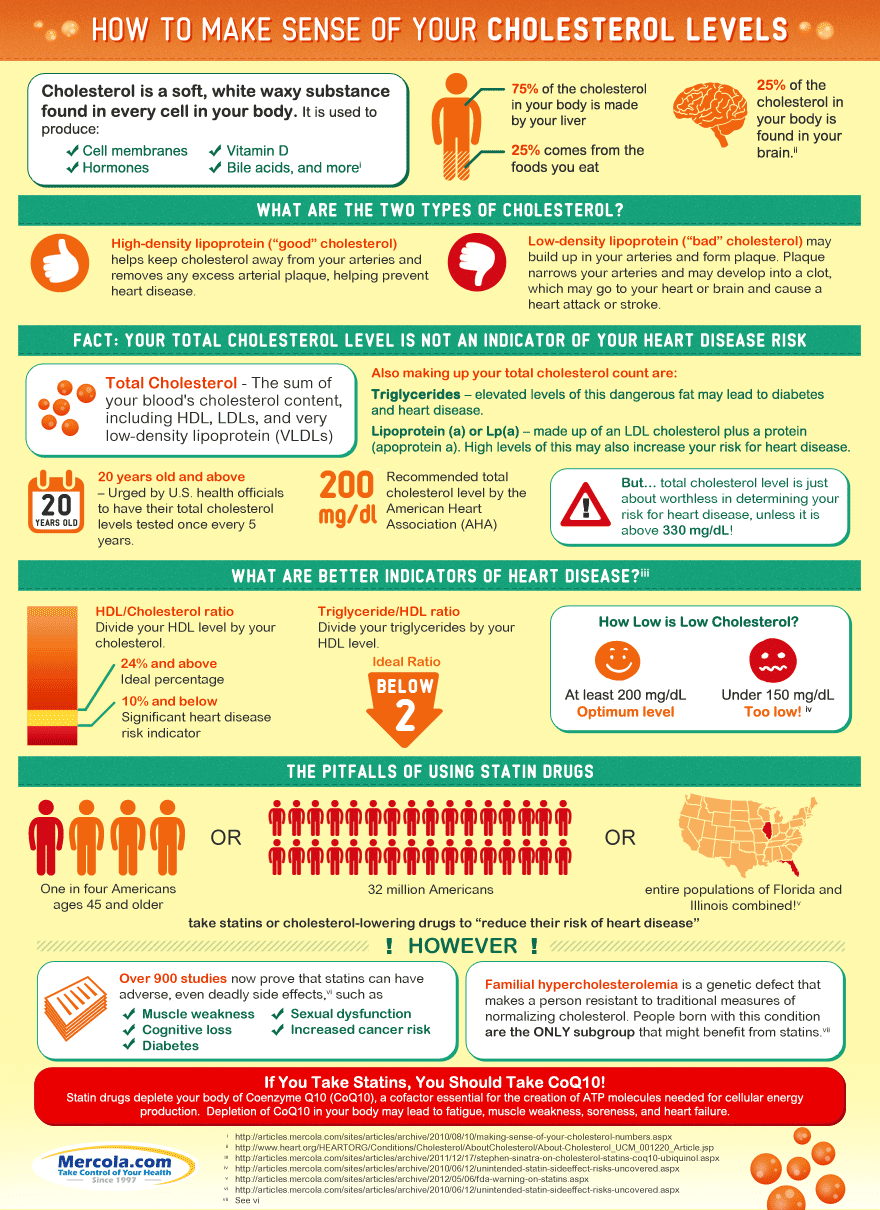
As a general rule, cholesterol-lowering drugs are not required or prudent for the majority of people — especially if both high cholesterol and longevity run in your family. Also keep in mind that your overall cholesterol level says very little about your risk for heart disease. For more information about cholesterol and what the different levels mean, take a look at the infographic above. As for evaluating your heart disease risk, the following tests will provide you with a far more accurate picture than your total cholesterol or LDL level alone:
|
HDL/Cholesterol ratio HDL percentage is a very potent heart disease risk factor. Just divide your HDL level by your total cholesterol. That percentage should ideally be above 24 percent. |
|
Triglyceride/HDL ratio You can also do the same thing with your triglycerides and HDL ratio. That percentage should be below 2. |
|
Large LDL particles are not harmful. Only small dense LDL particles can potentially be a problem, as they can squeeze through the lining of your arteries. If they oxidize, they can cause damage and inflammation. Some groups, such as the National Lipid Association, are now starting to shift the focus toward LDL particle number instead of total and LDL cholesterol, in order to better assess your heart disease risk. Once you know your particle size numbers, you and your doctor can develop a more customized program to help manage your risk. |
|
Your fasting insulin level Any meal or snack high in carbohydrates like fructose and refined grains generates a rapid rise in blood glucose and then insulin to compensate for the rise in blood sugar. The insulin released from eating too many carbs promotes fat accumulation and makes it more difficult for your body to shed excess weight. Excess fat, particularly around your belly, is one of the major contributors to heart disease. |
|
Your fasting blood sugar level Studies have shown that people with a fasting blood sugar level of 100-125 mg/dl had a nearly 300 percent increased higher risk of having coronary heart disease than people with a level below 79 mg/dl. |
|
Your iron level Iron can be a very potent oxidative stress, so if you have excess iron levels you can damage your blood vessels and increase your risk of heart disease. Ideally, you should monitor your ferritin levels and make sure they are not much above 80 ng/ml. The simplest way to lower them if they are elevated is to donate your blood. If that is not possible you can have a therapeutic phlebotomy and that will effectively eliminate the excess iron from your body. |
Sources and References: see below.
Recommended articles by Dr. Joseph Mercola:
- How LED Lighting May Compromise Your Health
- Depression is Now the No. 1 Cause of Illness and Disability Worldwide
- Essential Oils Can Help Ease Symptoms of ADHD
- Medical Errors: Still the Third Leading Cause of Death
- Plants Are Smarter Than You Think
- Photobiology: How Therapeutic Use of Full-Spectrum Light Can Improve Your Health
- Scientific Links Between Processed Foods and Depression
- How Sugar Harms Your Brain Health and Drives Alzheimer’s Epidemic
- The Health Benefits of Intermittent Fasting
- Can a Hug a Day Keep Infection Away?
- The Magic Healing Power of Mushrooms
- The Science of Healing Thoughts
- 13 Mind-Body Techniques That Can Help Ease Pain and Depression
About the author:
 Born and raised in the inner city of Chicago, IL, Dr. Joseph Mercola is an osteopathic physician trained in both traditional and natural medicine. Board-certified in family medicine, Dr. Mercola served as the chairman of the family medicine department at St. Alexius Medical Center for five years, and in 2012 was granted fellowship status by the American College of Nutrition (ACN).
Born and raised in the inner city of Chicago, IL, Dr. Joseph Mercola is an osteopathic physician trained in both traditional and natural medicine. Board-certified in family medicine, Dr. Mercola served as the chairman of the family medicine department at St. Alexius Medical Center for five years, and in 2012 was granted fellowship status by the American College of Nutrition (ACN).
While in practice in the late 80s, Dr. Mercola realized the drugs he was prescribing to chronically ill patients were not working. By the early 90s, he began exploring the world of natural medicine, and soon changed the way he practiced medicine.
In 1997 Dr. Mercola founded Mercola.com, which is now routinely among the top 10 health sites on the internet. His passion is to transform the traditional medical paradigm in the United States. “The existing medical establishment is responsible for killing and permanently injuring millions of Americans… You want practical health solutions without the hype, and that’s what I offer.”
Visit Mercola.com for more information, or read Dr. Mercola’s full bio and résumé here.
- 1 Health.gov 2015 Dietary Guidelines
- 2, 6 Health.gov, 2015 DGAC December 15, 2014 (PDF)
- 3 Health.gov, Dietary Guidelines 2015
- 4 CNN January 7, 2016
- 5 PBS January 7, 2016
- 7, 18 BMJ 2016;353:i1246
- 8 The Atlantic April 14, 2016
- 9, 30 New York Times April 13, 2016
- 10 Arklatex April 13, 2016
- 11 WebMD April 12, 2016
- 12 TIME April 12, 2016
- 13 Newswise April 12, 2016
- 14 Huffington Post April 13, 2016
- 15 Science Daily April 12, 2016
- 16 Newsweek April 19, 2017
- 17 Scientific American April 19, 2017
- 19, 20 DrCate.com, Deep Nutrition
- 21 Washington Post June 16, 2015
- 22 BMJ 2013;346:e8707
- 23 Bull N Y Acad Med. 1968 Aug; 44(8): 1012–1020.
- 24 Circulation. 1969; 40: II-1-II-63
- 25 The Lancet September 28, 1968, Volume 292, No. 7570, p693-700
- 26 ClinicalTrials.gov October 27, 1999
- 27 BMJ 2013;347:f6340
- 28 Annals of Internal Medicine March 18, 2014
- 29 BMJ 2015;351:h3978
- 31 CDC.gov, Prescription Cholesterol-Lowering Medication Use in Adults, 2003-2012 (PDF)
- 32 American Heart Association, 2013 CV Risk Calculator
- 33 Drsinatra.com November 13, 2013
- 34, 35 CNN April 18, 2017
- 36 JAMA 2016;316(19):2008-2024
- 37 Expert Rev Clin Pharmacol. 2015 Mar;8(2):201-10.
- 38 Archives of Internal Medicine 2010;170(12):1024-1031
- 39 The Telegraph June 13, 2016
- 40 Lovastatin – FDA prescribing information, side effects and uses. (2016). Drugs.com. Retrieved 20 June 2016
- 41 FDA Expands Advice on Statin Risks. (2016). Fda.gov. Retrieved 20 June 2016
- 42 J Med Food. 2013 Nov;16(11):965-7
- 43 Cancer Epidemiol Biomarkers Prev. 2013 Sep;22(9):1529-37.
- 44 Neuro Endocrinol Lett. 2011;32(5):688-90
- 45 Statin therapy decreases myocardial (heart) function.. (2016). Greenmedinfo.com. Retrieved 20 June 2016
[pro_ad_display_adzone id=”110027″]