Guest Writer for Wake Up World
Few people are truly aware of the importance of a balanced gut for their overall health and wellbeing. Some may even be unaware that we have a teeming community of microbes inside us! This unseen population of trillions of microbes comprises the gastrointestinal ecosystem that is known as your gut microbiome made up of bacteria, viruses, fungi, and more. The gut “flora” (microbes) is referred to by scientists as microbiota.
[pro_ad_display_adzone id=”110028″]
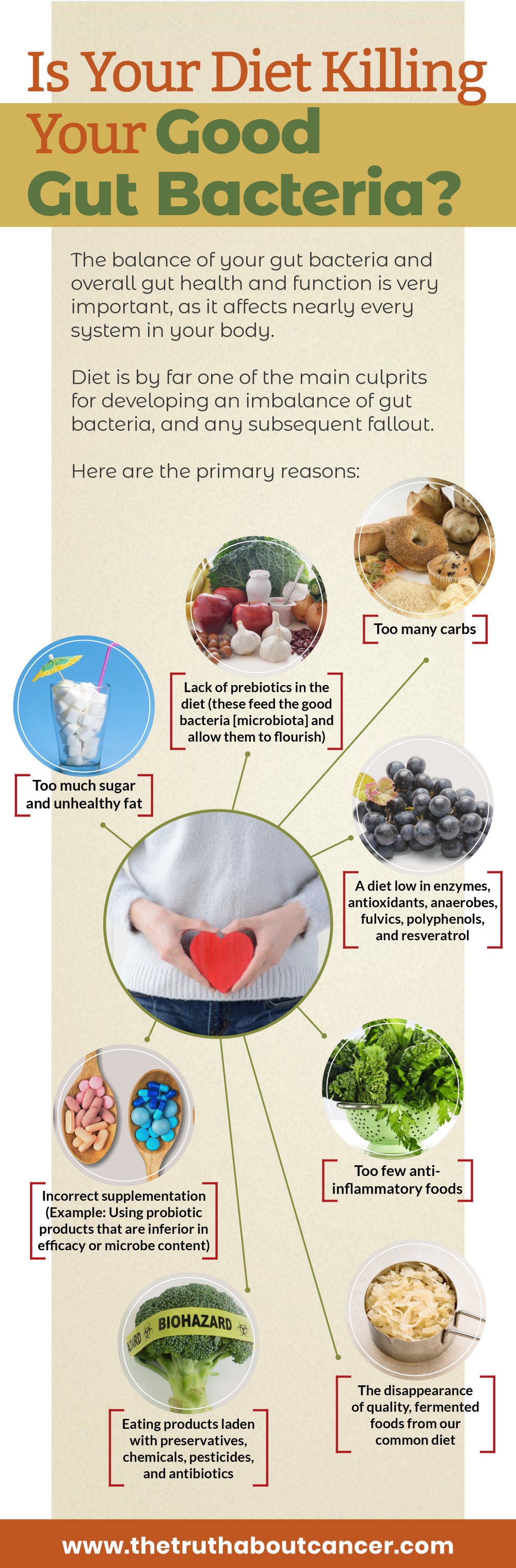
The balance of your microbiota, and overall microbiome health and function, is extremely important, affecting nearly every system in your body. An imbalance (often referred to as dysbiosis) of the gut microbiome and microbiota has been connected to many issues in the body including:
- Allergies
- Depression
- Autism
- Obesity and weight gain
- Digestive disorders (GERD, IBS, etc.)
- Yeast overgrowth
- Compromised immunity
and much more!
What Is an Imbalance of Microbiota?
A “balanced” microbiome refers to the optimum synergy in the symbiotic relationship between the microbes themselves, the function of each, and how those processes relate to your body. Generally stated, this is achieved by having: 1) a great diversity of microbiota, and 2) optimal levels of each microbe.
If one type of microbe is allowed to either gain the upper hand or be depleted, there can be repercussions for your health. Examples of such consequences would include fungi (yeast) being able to flourish, leading to yeast overgrowth. A depletion in yeast can also cause issues. Not enough yeast can lead to a lack of enzymes and less nutrients absorption. Then, there are bacteria, such as Clostridium and Fusobacterium, that in some circumstances may become harmful pathogens.
The microbiome really is that delicate of an ecosystem. Unfortunately, it’s all too easy to mess with its balance. In fact, one animal study found that a high-fat, high-sugar diet (the typical Western diet) measurably “shifted the structure of the microbiota within a single day.”
If we’re ignorant of the damage we’re doing, we can inadvertently pile on the damage, through various means. This can create the perfect storm of imbalance that leads to weakened immune function, and other states that have been directly connected to disease or, at minimum, poor health.
4 Common Ways Your Gut Microbiome (Gut Flora) May Become Imbalanced
Here are four of the most common ways you may be throwing your own microbiome and microbiota out of balance.
Risk Factor #1: Using Splenda (sucralose)
There’s been controversy about sweeteners for decades. Usually it’s aspartame (NutraSweet or Equal) and saccharin that get most of the flack, publicly. However, sucralose is not immune to examination or the need for caution. Splenda is marketed as being close to nature and being “made” from real sugar. The reality is sucralose is the result of chlorinating sucrose (sugar). So, it may start out as sugar, but what it becomes sure isn’t natural.
Think of it like butter versus margarine. You take a healthy, fairly inert oil and you hydrogenate it to make margarine, and all of a sudden, it’s not inert or healthy at all!
The process of making sucralose binds chlorine to the sugar molecule, meaning you are intentionally ingesting chlorine, which is a known poison. The processes the body goes through to deal with this toxic substance creates other chemical reactions that are harmful to the body.
On top of this, in order to prevent the chlorine from detaching, so to speak, other spectacularly harmful chemicals are added to the mix. You don’t see these on the ingredients list because they are in amounts that do not require labeling, by law. The chemicals you may be ingesting along with your sucralose include:
- acetone
- acetic acid
- acetyl alcohol
- ammonium chloride
- benzene
- ethyl alcohol
- formaldehyde
- hydrogen chloride
- lithium chloride
- methanol
- sulfuryl chloride
In fact, back in 1976, the creators of Splenda have been reported as stating,
Sucralose is made from sugar, but is derived from sucrose (sugar) through a process that selectively substitutes three atoms of chlorine for three hydrogen-oxygen groups on the sucrose molecule. No artificial sweetener made in the laboratory is going to be neither natural to the body nor safer than unprocessed sugar.”
In a 2008 study with rats consuming sucralose, negative effects were noted to the microbiome and microbiota. After 12 weeks of recovery (not taking the sucralose), the good bacteria and anaerobes were still notably decreased – by as much as 53.9%.
Not only that, the rats that had the lowest doses gained the most weight, though food quantities did not vary. It’s worth noting that an unbalanced microbiome has also been connected to weight gain. The possibility arises that sucralose’s ability to affect the microbiome plays a part in this phenomenon.
The researchers of this same study also observed a significant effect on important proteins involving nutrient absorption and medicines. Sucralose, therefore, is not as harmless as Big Food marketing departments would have you believe.
Risk Factor #2: Alcohol Consumption
In addition to harming many bodily systems, alcohol also damages your gut microbiome. It can lead to alterations of the gut flora (i.e. small intestinal bacterial overgrowth).
In 2009, a study looking at the effect of alcohol on microbiota found significant dysbiosis (microbial imbalance) with the alcohol-fed rats. In contrast, the imbalance was prevented by administering the probiotic (beneficial bacteria), Lactobacillus. The power of probiotics!
Other studies have demonstrated specific harmful bacteria overgrowth due to alcohol. Conversely, the probiotic Lactobacilli was seen to be severely depleted.
One specific condition associated with alcohol consumption is that of dysbiosis of the small intestine: SIBO – Small Intestine Bacteria Overgrowth. Typically the large intestine contains the greater amounts of bacteria, and a much lower number in the smaller. The problem with SIBO is complex, but to put it simply, the extra bacteria in the small intestine are able to consume nutrients that should be absorbed by the body. This can lead to malnourishment. Also, this breakdown of nutrients can lead to bowel problems and gas.
Many studies looking at the alcohol-microbiome link have been with high amounts of alcohol, looking at dysbiosis and alcoholism. However, a human study by Dr. Scott Gabbard and team at the Dartmouth-Hitchcock Medical Center and the Mayo Clinic looked at moderate consumption. They found that even a small amount of alcohol could impact gut health.
Suffice to say, if you know you have a gut imbalance, you want to avoid alcohol while you replenish and rebalance with a good probiotic foods and/or a supplement.
Risk Factor #3: Poor Diet
Diet is by far one of the main culprits for developing an imbalance of microbiota, and any subsequent fallout. Here are the primary reasons:
- Too much sugar and (unhealthy) fat
- Too many carbs
- Too few anti-inflammatory foods, such as fresh, green leafy vegetables
- A diet low in enzymes, antioxidants, anaerobes, fulvics, polyphenols, and resveratrol
- Eating products laden with preservatives, chemicals, pesticides, and antibiotics
- The disappearance of quality fermented foods from our common diet
- Lack of prebiotics in the diet (these feed the good bacteria [microbiota] and allow them to flourish)
- Incorrect supplementation (ie: using probiotic products that are inferior in efficacy or microbe content, such as mass market yogurts)
Risk Factor #4: Using Antibiotics
If there was a countdown, this would be the dramatic finish because antibiotics are likely the worst cause of an imbalanced gut. Especially if used regularly, and in combination with all the above.
It’s simple: antibiotics are life-saving medicines that kill bacteria that in the past, in particular, would have been too much for the body to heal on its own. Nowadays there is a tendency to use these miracle meds even when there is not a life-threatening illness, whether for speed of recovery or to avoid the chance of an infection getting to that level.
So we take them. Even when at times we’re playing a 50/50 game with our ailment actually being a virus. Either way, the antibiotics do their job and wipe out bacteria in our system. The problem then arises in the gut.
As you now know, the gut microbiome is a delicate balance of organisms. However, the “good” and “bad” bacteria are all the same to antibiotics. When you take antibiotics, both are killed indiscriminately leaving your microbiome at risk of other microbes taking over, including resistant bacteria.
Overgrowth of yeast is probably the most well-known result of taking antibiotics. We need yeasts for our gastrointestinal ecosystem, but, as with everything else, in the right balance. There are bacteria in the gut that feed off killing the yeasts and fungi. There are those that, in interacting with the yeast, create enzymes and other chemicals and compounds that promote health.
When yeast is allowed to grow out of control, say, when antibiotics have wiped out these aforementioned bacteria, it can lead to health problems. Yeast overgrowth is under suspicion for being at the root of disease, as well as many common health issues such as urinary tract infections (UTIs), respiratory infections, and sinus infections.
A study on the effects of taking the antibiotic Ciprofloxacin found that up to a third of bacterial varieties were killed with just one dose. While most of the test study subjects had a rebalanced flora by the 4th week following treatment, some did not even after 6 months.
Someone who is prone to having a lengthy recovery time should definitely be wary of taking too many antibiotics.
Anyone taking antibiotics should be aware of the potential effects and be certain to:
- Take a quality probiotic in conjunction with the medicine, and
- Follow up a course of antibiotics with a proactive plan to replenish the microbiota through diet, avoiding alcohol and sucralose, as well as continuing with a top drawer probiotic that ideally has fermented enzymes
3 Things That PROMOTE Good, Healthy Gut Bacteria
#1. Fermented Foods
The remedy seems pretty simple there… avoid the things that cause the imbalance, and start including good sources of those that help it.
Take fermented foods. For centuries, different cultures have all had their own versions of fermented foods. These cultural treats are not simply tasty, they served a purpose – mainly that of preserving foods before there was adequate refrigeration, and for travel. However, whether by design of accident, there’s much more to it than that.
Fermented foods and substances actually contain a wide range of microbe goodness that is incredibly beneficial for your microbiome. A diverse set of microbiota equals a happy gut. Eating a diverse range of fermented foods and substances will give you a better balanced microbiome.
It begins with the pre-digestion that occurs in the fermenting. The sugars and starches are broken down by probiotics and yeasts. The end result is an array of probiotics that your gut loves, as well as lactic acid.
#2. Anaerobes
The benefits of eating fermented foods and substances is largely due to anaerobes, which are a specialized microbe that assist in the fermentation process, at the same time creating bioactive compounds. These compounds themselves have many benefits, including properties that are antioxidant, antihypertensive, and even anti-cancer. Best of all, anaerobes make the nutrients in fermented foods, and within your own digestive system, more bioavailable to you. This means more is absorbed and utilized by the body.
#3. Fulvic
Something else we used to consume more of in ancient times are fulvic and humic acids. These substances are promoters of a balanced microbiome and help your body to absorb probiotics. Organic vegetables grown directly in the soil are high in fulvic acid.
It is thought the main reason fulvics are so beneficial for our microbiome and health is that they form bonds with bioactive molecules, acting as a carrier for them. Digestive disorders such as leaky gut (food, pathogens, and other particles are able to pass through the intestinal lining into the bloodstream), SIBO, and IBS can be supported or potentially avoided with the use of good fulvics.
References:
- What is the Gut Microbiota? What is the Human Microbiome?
- Role of the Gut Microbiota in Defining Human Health
- Any Role for probiotics in the therapy or prevention of autoimmune diseases? Up-to-date review
- Therapeutic Manipulation of Immune Tolerance in Allergic Disease
- Allergy and the Gastrointestinal System
- Can the Bacteria in Your Gut Explain Your Mood?
- Serotonin, Tryptophan Metabolism and the Brain-Gut-Microbiome Axis
- The Gut-Brain Axis: Interactions Between Enteric Microbiota, Central and Enteric Nervous System
- The Role of Gut Microbiota in the Development of Type 1, Obesity and Type 2 Diabetes Mellitus
- The Core Gut Microbiome, Energy Balance and Obesity.
- Microecology, Obesity, and Probiotics.
- How Gut Bacteria Help Make Us Fat and Thin
- The Effect of Diet on the Human Gut Microbiome: A Metagenomic Analysis in Humanized Gnotobiotic Mice
- ‘Gut health’: A New Objective in Medicine?
- What Are Probiotics?
- Saccharomyces boulardii Stimulates Intestinal Immunoglobulin A Immune Response to Clostridium difficile Toxin A in Mice
- Escherichia, Klebsiella, Enterobacter, Serratia, Citrobacter, and Proteus
- Gut microbiota and Clostridium difficile infections
- Lymphoid Tissue Genesis Induced by Commensals through NOD1 Regulates Intestinal Homeostasis.
- Probiotics as Efficient Immunopotentiators: Translational Role in Cancer Prevention
- Constitution of the World Health Organization
- Review article: Alcohol and gut microbiota – the possible role of gut microbiota modulation in the treatment of alcoholic liver disease.
- The Effect of Diet on the Human Gut Microbiome: A Metagenomic Analysis in Humanized Gnotobiotic Mice
- All about Sucralose – Your Questions Answered
- WEIRD SCIENCE: How Splenda Was Discovered
- Butter vs. Margarine
- Butter Unlikely to Harm Health, but Margarine could be Deadly
- Non-Caloric Artificial Sweeteners and the Microbiome: Findings and Challenges
- Non-Caloric Artificial Sweeteners and the Microbiome: Findings and Challenges
- Research Review: Is Splenda safe?
- Splenda Alters Gut Microflora and Increases Intestinal P-Glycoprotein and Cytochrome P-450 in Male Rats.
- Intestinal Dysbiosis: A Possible Mechanism of Alcohol-Induced Endotoxemia and Alcoholic Steatohepatitis in Rats
- Moderate Alcohol Consumption is Associated with Small Intestinal Bacterial Overgrowth, Study Finds
- The History and Health Benefits of Fermented Food
- The Definitive Guide to Traditional Food Preparation and Preservation
- Inhibition of Escherichia Coli O157:H7 Attachment by Interactions between Lactic Acid Bacteria and Intestinal Epithelial Cells.
- Anaerobes as Sources of Bioactive Compounds and Health Promoting Tools.
- Dietary Fructose and Intestinal Barrier: Potential Risk Factor in the Pathogenesis of Nonalcoholic Fatty Liver Disease.
- Optimizing Digestive Health
- Isolation and Characterization of Putative Probiotic Bacterial Strain, Bacillus Amyloliquefaciens, from North East Himalayan Soil Based on In Vitro and In Vivo Functional Properties.
- Discover Why Fulvic Acid is So Good for Your Gut, Brain & Skin
- Influence of Antibiotic Exposure in the Early Postnatal Period on the Development of Intestinal Microbiota.
- Risk Assessment of Ciprofloxacin, Flavomycin, Olaquindox and Colistin Sulfate based on Microbiological Impact on Human Gut Biota.
- Specificity of Polysaccharide Use in Intestinal Bacteroides Species Determines Diet-Induced Microbiota Alterations.
- A Primal Primer: Prebiotics
- Dietary Modulation of the Human Colonic Microbiota: Introducing the Concept of Prebiotics
- Probiotics in Man and Animals
- Probiotic Escherichia coli Nissle 1917 Inhibits Leaky Gut by Enhancing Mucosal Integrity.
- The Pervasive Effects of an Antibiotic on the Human Gut Microbiota, as Revealed by deep 16S rRNA Sequencing.
- Antibiotics Kill Your Body’s Good Bacteria, Too, Leading to Serious Health Risks
- Otorhinolaryngology (ENT) in Minnesota
- Nutritional Yeast: The Good and the Bad and What You Need to Know If You Seek a Stronger Immune System
Originally published at The Truth About Cancer and reproduced here with permission.
About the author:
 Ty Bollinger is a health freedom advocate, cancer researcher, former competitive bodybuilder and author. After losing several family members to cancer, he refused to accept the notion that chemotherapy, radiation, and surgery were the most effective treatments available for cancer patients. He began a quest to learn all he possibly could about alternative cancer treatments and the medical industry. What he uncovered was shocking. There is ample evidence to support the allegation that the “war on cancer” is largely a fraud and that multinational pharmaceutical companies are “running the show.” Ty has now made it his life mission to share the most remarkable discovery he made on his quest: the vast majority of all diseases, including cancer, can be easily prevented and even cured without drugs or surgery.
Ty Bollinger is a health freedom advocate, cancer researcher, former competitive bodybuilder and author. After losing several family members to cancer, he refused to accept the notion that chemotherapy, radiation, and surgery were the most effective treatments available for cancer patients. He began a quest to learn all he possibly could about alternative cancer treatments and the medical industry. What he uncovered was shocking. There is ample evidence to support the allegation that the “war on cancer” is largely a fraud and that multinational pharmaceutical companies are “running the show.” Ty has now made it his life mission to share the most remarkable discovery he made on his quest: the vast majority of all diseases, including cancer, can be easily prevented and even cured without drugs or surgery.
For more information, visit:
[pro_ad_display_adzone id=”110027″]