Guest writer for Wake Up World
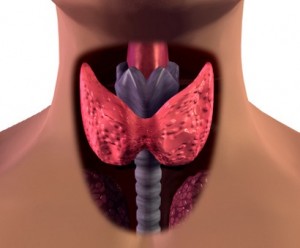
When most people think of the thyroid, the first thing that may come to mind is an image of a simple, obscure gland located somewhere in the neck. The thyroid is often seen as serving unknown functions as it is rarely discussed in popular press. Likewise, it’s not at all surprising that few understand its exact function and just how important it is to our overall health, wellness and vitality.
In this article we will briefly cover what the thyroid is and its functions, and discuss the 5 most common thyroid disorders today.
Thyroid Functions
The thyroid is an endocrine gland that produces and directs various hormones in the body. The health of the thyroid is paramount to overall well being, playing a vital role in cell growth, metabolism, and energy levels. The thyroid produces two major primary hormones called triiodothyronine (T3) and thyroxine (T4). T3 is the more bio active version of the hormone, while T4 is considered the less active, storage form. Surprisingly, the thyroid outputs roughly 20 times more T4 than T3.
Lesser known, the thyroid’s secondary role is the production of the calcium-regulating hormone calcitonin, which regulates and balances blood calcium levels and calcium deposition in bones.
Thyroid-stimulating hormone (TSH) released from the pituitary helps regulate the hormonal output and balance of the thyroid, regulating how much of the primary T3 and T4 hormones are manufactured and released. Before all of that happens, the TSH release is first stimulated by the area of the brain that controls neuroendocrine and central nervous system function. The hypothalamus then sends out its own stimulatory hormone called thyrotropin-releasing hormone (TRH).
The 5 Most Common Thyroid Disorders
Thyroid disorders affect millions of Americans yearly, and the number of people afflicted continues to grow with each passing year. Growing research data suggests that aside from the genetic origin of the various clinically significant thyroid disorders, much of the causation is likely due to lifestyle factors such as constant exposure to a toxic environment, the consumption of chemically-laden food and water, as well as a deficiency of certain nutrients.
Though thyroid disorders affect men and women alike – up to 20 million Americans – the predominance of disorders are found in women, upwards of 80%. 1 in 8 women will experience some type of thyroid disorder in their lives. [1]
1. Hyperthyroidism
Hyperthyroidism is defined as an overactive thyroid gland which produces an overabundance of T3/T4 hormones. Symptoms of hyperthyroidism include goiter, heart palpitations, anxiety, excess sweating, diarrhea, weight loss, and muscle weakness. Causes are as diverse as its symptoms, but nevertheless are important to understand. Autoimmunity of the thyroid often leads to Grave’s Disease, a disorder that results in an overactive thyroid. Also, nodule formation and/or goiter formation in the thyroid, leading to inhibition of necessary hormone feedback loops, contributes to excess production of thyroid hormones. Excess dietary iodine intake can also increase risk for hyperthyroidism.
Conventional approaches to hyperthyroidism include beta blockers, radioactive iodine, and surgery. Natural approaches are numerous and often boil down to one thing: diet. Eliminating goitrogenic foods may be helpful, as would removing fluoride, bromine, and chlorine from water via a high-quality filtration system. Reducing dietary gluten and dairy casein may also help protect the thyroid gland in sensitive individuals. Nascent iodine, lithium orotate, probiotics, vitamin D3, omega -3 fats, L -dopa (mucuna pruriens), and L-tyrosine are possible helpful supplements that can be taken for supporting thyroid health. Make sure to get plenty of sleep to recharge the thyroid, and avoid synthetic chemicals whenever possible. Deep breathing meditation and general relaxation may also be helpful for reducing stress associated with the thyroid. [2] [3]
2. Hypothyroidism
On the opposite end of the spectrum, an underactive thyroid which produces inadequate amounts of T3/T4 thyroid hormones is defined as hypothyroidism. Symptoms include tiredness, excessive weight gain, cold intolerance, baldness, depression, dry skin/hair/nails, and irritability. Common causes include a congenital abnormality (thyroid deficiency from birth), autoimmune inflammation of the thyroid such as Hashimoto’s thyroiditis, nutritional iodine deficiency, TSH hormone deficiency via pituitary gland abnormality, heavy metal toxicity, and dysbiosis (imbalance of good vs. bad bacteria).
Common treatment is the injection of synthetic thyroid hormone called Levothyroxine to boost hormone levels. With the exception of increasing exercise, the natural action steps to reduce risk for hypothyroidism are exactly the same for hyperthyroidism. [4] Exercise may help boost thyroid hormones, providing support for a sluggish, underactive gland.
3. Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune disorder whereby the thyroid gland is attacked by the immune system in response to antibodies produced by exposure to an allergen. This reacts with the cells and tissues of the thyroid, causing inflammation and destruction of the gland, ultimately leading to hyperthyroidism followed by hypothyroidism. Fatigue, cold intolerance, constipation, goiter, weight gain, paleness/puffiness in face, sleepiness, joint/muscular pain, dry/brittle hair, and depression are common symptoms. [5]
Medical experts postulate that viruses, bacteria, and other foreign substances initiate the process of Hashimoto’s thyroiditis autoimmunity. Iodine deficiency in conjunction with fluoride/chlorine/bromine exposure may also be a contributing factor. A gluten allergy may be another hidden culprit behind Hashimoto’s disease. Vitamin D deficiency and dysbiosis are also common concerning factors. Conventional and natural approaches are similar to that of hypothyroidism.
4. Grave’s Disease
Similar to Hashimoto’s disease, Grave’s disease is an autoimmune disorder whereby the thyroid gland is attacked by the immune system from antibodies produced in response to an allergen. This confuses the cells of the thyroid, causing inflammation and the overproduction of T3/T4 thyroid hormones, eventually leading to an overactive thyroid (hyperthyroid). [6]
Symptoms include anxiety, heart palpitations, goiter, hand tremors, weight loss, insomnia, irritability, muscle weakness, diarrhea, heat intolerance, and eye problems. The causes are very similar to that of Hashimoto’s disease. Approaches are generally the same as with general hyperthyroidism and include beta blockers, anti -thyroid medications such as methimazole and propylthiouracil, radioactive iodine , surgery, and avoiding goitrogenic foods.
5. Thyroiditis
Thyroiditis is defined as the swelling or inflammation of the thyroid gland. There are a few main types:
- Hashimoto’s thyroiditis
- Postpartum thyroiditis potentially caused by autoimmune response, often in two phases:
- The first phase occurs months 1 through 4 postpartum, resulting in hyperthyroidism.
- The second phase generally lasts from months 4 through 8 postpartum and often results in a hypothyroid condition due to the exhaustion of thyroid hormones in the earlier phase. Recovery usually happens naturally 12- 18 months postpartum.
- Silent/painless thyroiditis, similar to postpartum but not related to birth.
- Subacute thyroiditis, similar to the others but causes pain in jaw/neck/ear, possibly from autoimmunity or infection.
Iodine deficiency in conjunction with fluoride/chlorine/bromine displacement may be an important contributing factor in thyroiditis. Gluten allergy, vitamin D deficiency, and dysbiosis may also be factors associated with the condition. Depending on the type of thyroiditis, medications usually vary depending on whether it presents initially with hyper - or hypothyroidism. [7]
– Dr. Edward F. Group III, DC, ND, DACBN, DCBCN, DABFM
References:
- American Thyroid Association. Thyroid Disease. Fact Sheet.
- Delitala G, Masala A, et al. Plasma prolactin response to L dopa TRH and metaclopramide in thyrotoxicosis. Biomedicine. 1976 Jul;25(5):173 6.
- NIH/NEMDS. Hyperthyroidism. National Institute of Health. Fact Sheet.
- JNIG/NEMDS. Hypothyroidism. Fact Sheet.
- NIH/NEMDS. Hashimoto’s Disease. Fact Sheet.
- NIH/NEMDS. Grave’s Disease. Fact Sheet.
- Office of Women’s Health/U.S. HHS. Thyroid disease. Fact Sheet.
Recommended articles by Dr. Group:
- 6 Things You Must Know About Colloidal Silver
- The 9 Best Herbs for Lung Cleansing and Respiratory Support
- 7 Best Foods to Support Kidney Function
- How to Flush the Liver
- Lung Cleansing With Peppermint Oil
- The Benefits of Organic Hemp Milk + How to Make Your Own
- Nine Shocking Dangers of Fluoride Exposure
- 12 Shocking Facts About the Dangers of Psychiatric Drugs
- Seven Facts You May Not Know About Coconut Oil
- 5 Dangerous Chemicals in Conventional Sunscreens
- How Colloidal Silver Combats Harmful Organisms
About the author:
 Dr. Edward F. Group III (DC, ND, DACBN, DCBCN, DABFM) founded Global Healing Center in 1998 and is currently the Chief Executive Officer. Heading up the research and development team, Dr. Group assumes a hands-on approach in producing new and advanced degenerative disease products and information.
Dr. Edward F. Group III (DC, ND, DACBN, DCBCN, DABFM) founded Global Healing Center in 1998 and is currently the Chief Executive Officer. Heading up the research and development team, Dr. Group assumes a hands-on approach in producing new and advanced degenerative disease products and information.
Dr. Group has studied natural healing methods for over 20 years and now teaches individuals and practitioners all around the world. He no longer sees patients but solely concentrates on spreading the word of health and wellness to the global community. Under his leadership, Global Healing Center, Inc. has earned recognition as one of the largest alternative, natural and organic health resources on the internet.
For more information, please visit Global Healing Center.

If you've found value in our articles, we invite you to support the release of our brand-new book, "Gratitude Practices for Kids: A Practical Guide for Adults to Instill a Spirit of Appreciation and Positivity in the Next Generation."
"Gratitude Practices for Kids" brings together over 25 innovative and accessible practices designed to enhance gratitude in everyday life. This comprehensive guide is backed by 17 scientific studies, ensuring each concept is grounded in research, underscoring our commitment to nurturing growth, emotional intelligence, and positive interactions between adults and children.
We encourage you to opt for the paperback version to celebrate this new release. Dive into its fresh pages away from digital distractions, allowing you to immerse yourself in the transformative practices it offers.
Over recent years, Wake Up World has faced significant online censorship, which has impacted our financial ability to operate. Moving into book publishing represents a strategic step to secure the ongoing funds needed to continue our mission. By purchasing Gratitude for Kids, you help us keep our content free and accessible to everyone, avoiding needing a paywall. With over 8,500 articles published in the last 13 years, we remain dedicated to keeping our valuable content open to all.